Related Research Articles

Gadolinium is a chemical element; it has symbol Gd and atomic number 64. Gadolinium is a silvery-white metal when oxidation is removed. It is a malleable and ductile rare-earth element. Gadolinium reacts with atmospheric oxygen or moisture slowly to form a black coating. Gadolinium below its Curie point of 20 °C (68 °F) is ferromagnetic, with an attraction to a magnetic field higher than that of nickel. Above this temperature it is the most paramagnetic element. It is found in nature only in an oxidized form. When separated, it usually has impurities of the other rare earths because of their similar chemical properties.

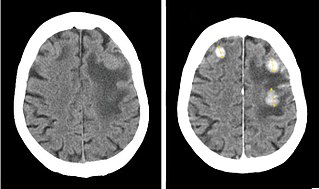
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes inside the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from computed tomography (CT) and positron emission tomography (PET) scans. MRI is a medical application of nuclear magnetic resonance (NMR) which can also be used for imaging in other NMR applications, such as NMR spectroscopy.

Radiography is an imaging technique using X-rays, gamma rays, or similar ionizing radiation and non-ionizing radiation to view the internal form of an object. Applications of radiography include medical and industrial radiography. Similar techniques are used in airport security,. To create an image in conventional radiography, a beam of X-rays is produced by an X-ray generator and it is projected towards the object. A certain amount of the X-rays or other radiation are absorbed by the object, dependent on the object's density and structural composition. The X-rays that pass through the object are captured behind the object by a detector. The generation of flat two-dimensional images by this technique is called projectional radiography. In computed tomography, an X-ray source and its associated detectors rotate around the subject, which itself moves through the conical X-ray beam produced. Any given point within the subject is crossed from many directions by many different beams at different times. Information regarding the attenuation of these beams is collated and subjected to computation to generate two-dimensional images on three planes which can be further processed to produce a three-dimensional image.

Radiology is the medical specialty that uses medical imaging to diagnose diseases and guide treatment within the bodies of humans and other animals. It began with radiography, but today it includes all imaging modalities. This includes technologies that use no ionizing electromagnetic radiation, such as ultrasonography and magnetic resonance imaging), as well as others that do use radiation, such as computed tomography (CT), fluoroscopy, and nuclear medicine including positron emission tomography (PET). Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.

Medical imaging is the technique and process of imaging the interior of a body for clinical analysis and medical intervention, as well as visual representation of the function of some organs or tissues (physiology). Medical imaging seeks to reveal internal structures hidden by the skin and bones, as well as to diagnose and treat disease. Medical imaging also establishes a database of normal anatomy and physiology to make it possible to identify abnormalities. Although imaging of removed organs and tissues can be performed for medical reasons, such procedures are usually considered part of pathology instead of medical imaging.

An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".
Radiocontrast agents are substances used to enhance the visibility of internal structures in X-ray-based imaging techniques such as computed tomography, projectional radiography, and fluoroscopy. Radiocontrast agents are typically iodine, or more rarely barium sulfate. The contrast agents absorb external X-rays, resulting in decreased exposure on the X-ray detector. This is different from radiopharmaceuticals used in nuclear medicine which emit radiation.
Iodinated contrast is a form of water-soluble, intravenous radiocontrast agent containing iodine, which enhances the visibility of vascular structures and organs during radiographic procedures. Some pathologies, such as cancer, have particularly improved visibility with iodinated contrast.

An arthrogram is a series of images of a joint after injection of a contrast medium, usually done by fluoroscopy or MRI. The injection is normally done under a local anesthetic such as Novocain or lidocaine. The radiologist or radiographer performs the study using fluoroscopy or x-ray to guide the placement of the needle into the joint and then injects around 10 ml of contrast based on age. There is some burning pain from the anesthetic and a painful bubbling feeling in the joint after the contrast is injected. This only lasts 20 – 30 hours until the Contrast is absorbed. During this time, while it is allowed, it is painful to use the limb for around 10 hours. After that the radiologist can more clearly see what is going on under your skin and can get results out within 24 to 48 hours.

Contrast-enhanced ultrasound (CEUS) is the application of ultrasound contrast medium to traditional medical sonography. Ultrasound contrast agents rely on the different ways in which sound waves are reflected from interfaces between substances. This may be the surface of a small air bubble or a more complex structure. Commercially available contrast media are gas-filled microbubbles that are administered intravenously to the systemic circulation. Microbubbles have a high degree of echogenicity. There is a great difference in echogenicity between the gas in the microbubbles and the soft tissue surroundings of the body. Thus, ultrasonic imaging using microbubble contrast agents enhances the ultrasound backscatter, (reflection) of the ultrasound waves, to produce a sonogram with increased contrast due to the high echogenicity difference. Contrast-enhanced ultrasound can be used to image blood perfusion in organs, measure blood flow rate in the heart and other organs, and for other applications.
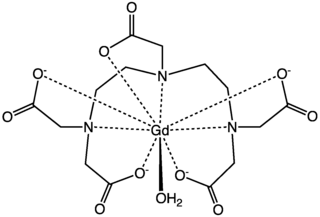
Gadopentetic acid, sold under the brand name Magnevist, is a gadolinium-based MRI contrast agent.
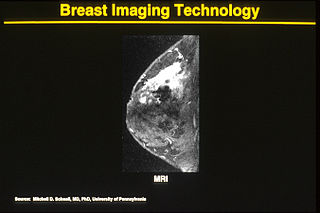
One alternative to mammography, breast MRI or contrast-enhanced magnetic resonance imaging (MRI), has shown substantial progress in the detection of breast cancer.

Echogenicity or echogeneity is the ability to bounce an echo, e.g. return the signal in medical ultrasound examinations. In other words, echogenicity is higher when the surface bouncing the sound echo reflects increased sound waves. Tissues that have higher echogenicity are called "hyperechoic" and are usually represented with lighter colors on images in medical ultrasonography. In contrast, tissues with lower echogenicity are called "hypoechoic" and are usually represented with darker colors. Areas that lack echogenicity are called "anechoic" and are usually displayed as completely dark.
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI). The most commonly used compounds for contrast enhancement are gadolinium-based contrast agents (GBCAs). Such MRI contrast agents shorten the relaxation times of nuclei within body tissues following oral or intravenous administration.

Cardiac magnetic resonance imaging, also known as cardiovascular MRI, is a magnetic resonance imaging (MRI) technology used for non-invasive assessment of the function and structure of the cardiovascular system. Conditions in which it is performed include congenital heart disease, cardiomyopathies and valvular heart disease, diseases of the aorta such as dissection, aneurysm and coarctation, coronary heart disease. It can also be used to look at pulmonary veins.

Iobitridol is a pharmaceutical drug used as an iodine-based radiocontrast agent in X-ray imaging. It is injected into blood vessels, joints, or body cavities such as the uterus, and filtered out by the kidneys. Its most common adverse effect is nausea. Severe allergic reactions are rare.

Preclinical imaging is the visualization of living animals for research purposes, such as drug development. Imaging modalities have long been crucial to the researcher in observing changes, either at the organ, tissue, cell, or molecular level, in animals responding to physiological or environmental changes. Imaging modalities that are non-invasive and in vivo have become especially important to study animal models longitudinally. Broadly speaking, these imaging systems can be categorized into primarily morphological/anatomical and primarily molecular imaging techniques. Techniques such as high-frequency micro-ultrasound, magnetic resonance imaging (MRI) and computed tomography (CT) are usually used for anatomical imaging, while optical imaging, positron emission tomography (PET), and single photon emission computed tomography (SPECT) are usually used for molecular visualizations.

Medical imaging in pregnancy may be indicated because of pregnancy complications, intercurrent diseases or routine prenatal care.
A specific branch of contrast-enhanced ultrasound, acoustic angiography is a minimally invasive and non-ionizing medical imaging technique used to visualize vasculature. Acoustic angiography was first developed by the Dayton Laboratory at North Carolina State University and provides a safe, portable, and inexpensive alternative to the most common methods of angiography such as Magnetic Resonance Angiography and Computed Tomography Angiography. Although ultrasound does not traditionally exhibit the high resolution of MRI or CT, high-frequency ultrasound (HFU) achieves relatively high resolution by sacrificing some penetration depth. HFU typically uses waves between 20 and 100 MHz and achieves resolution of 16-80μm at depths of 3-12mm. Although HFU has exhibited adequate resolution to monitor things like tumor growth in the skin layers, on its own it lacks the depth and contrast necessary for imaging blood vessels. Acoustic angiography overcomes the weaknesses of HFU by combining contrast-enhanced ultrasound with the use of a dual-element ultrasound transducer to achieve high resolution visualization of blood vessels at relatively deep penetration levels.

Focused ultrasound for intracrainial drug delivery is a non-invasive technique that uses high-frequency sound waves to disrupt tight junctions in the blood–brain barrier (BBB), allowing for increased passage of therapeutics into the brain. The BBB normally blocks nearly 98% of drugs from accessing the central nervous system, so FUS has the potential to address a major challenge in intracranial drug delivery by providing targeted and reversible BBB disruption. Using FUS to enhance drug delivery to the brain could significantly improve patient outcomes for a variety of diseases including Alzheimer's disease, Parkinson's disease, and brain cancer.
References
- ↑ "contrast agent" at Dorland's Medical Dictionary
- ↑ Thomson K, Varma D (2010). "Safe use of radiographic contrast media". Australian Prescriber. 33: 19–22. Archived from the original on 2011-03-17.
{{cite journal}}: CS1 maint: unfit URL (link) - ↑ "MR Contrast Agents". 2014.
- ↑ Postema M, Schmitz G (2006). "Bubble dynamics involved in ultrasonic imaging". Expert Review of Molecular Diagnostics. 6 (3): 493–502. doi:10.1586/14737159.6.3.493.