Electrocardiography is the process of producing an electrocardiogram, a recording of the heart's electrical activity. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances, inadequate coronary artery blood flow, and electrolyte disturbances.

A premature ventricular contraction (PVC) is a common event where the heartbeat is initiated by Purkinje fibers in the ventricles rather than by the sinoatrial node. PVCs may cause no symptoms or may be perceived as a "skipped beat" or felt as palpitations in the chest. PVCs do not usually pose any danger.

Palpitations are perceived abnormalities of the heartbeat characterized by awareness of cardiac muscle contractions in the chest, which is further characterized by the hard, fast and/or irregular beatings of the heart.
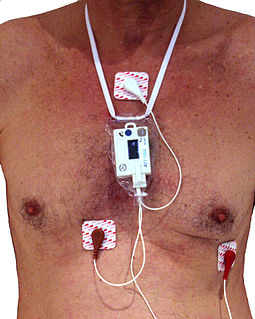
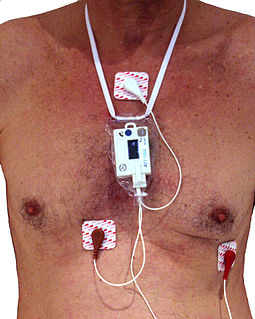
In medicine, a Holter monitor is a type of ambulatory electrocardiography device, a portable device for cardiac monitoring for at least 24 hours.

Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia. Atrial flutter is characterized by a sudden-onset (usually) regular abnormal heart rhythm on an electrocardiogram (ECG) in which the heart rate is fast. Symptoms may include a feeling of the heart beating too fast, too hard, or skipping beats, chest discomfort, difficulty breathing, a feeling as if one's stomach has dropped, a feeling of being light-headed, or loss of consciousness.

Ventricular tachycardia is a fast heart rate arising from the lower chambers of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.

A cardiac stress test is a cardiological test that measures the heart's ability to respond to external stress in a controlled clinical environment. The stress response is induced by exercise or by intravenous pharmacological stimulation.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

A heart rate monitor (HRM) is a personal monitoring device that allows one to measure/display heart rate in real time or record the heart rate for later study. It is largely used to gather heart rate data while performing various types of physical exercise. Measuring electrical heart information is referred to as electrocardiography.

Transposition of the great vessels (TGV) is a group of congenital heart defects involving an abnormal spatial arrangement of any of the great vessels: superior and/or inferior venae cavae, pulmonary artery, pulmonary veins, and aorta. Congenital heart diseases involving only the primary arteries belong to a sub-group called transposition of the great arteries (TGA), which is considered the most common congenital heart lesion that presents in neonates.

Atrioventricular block is a type of heart block that occurs when the electrical signal traveling from the atria, or the upper chambers of the heart, to ventricles, or the lower chambers of the heart, is impaired. Normally, the sinoatrial node produces an electrical signal to control the heart rate. The signal travels from the SA node to the ventricles through the atrioventricular node. In an AV block, this electrical signal is either delayed or completely blocked. When the signal is completely blocked, the ventricles produce their own electrical signal to control the heart rate. The heart rate produced by the ventricles is much slower than that produced by the SA node.

Variant angina, and less commonly Prinzmetal angina,vasospastic angina, angina inversa, coronary vessel spasm, or coronary artery vasospasm, is a syndrome typically consisting of angina in contrast to stable angina which is generally triggered by exertion or intense exercise, commonly occurs in individuals at rest or even asleep and is caused by vasospasm, a narrowing of the coronary arteries due to contraction of the heart's smooth muscle tissue in the vessel walls. In comparison, stable angina is due to the permanent occlusion of these vessels by atherosclerosis.

Left bundle branch block (LBBB) is a conduction abnormality in the heart that can be seen on an electrocardiogram (ECG). In this condition, activation of the left ventricle of the heart is delayed, which causes the left ventricle to contract later than the right ventricle.
Cardiovascular technologists are health professionals that deal with the circulatory system.

Cardiac monitoring generally refers to continuous or intermittent monitoring of heart activity, generally by electrocardiography, with assessment of the patient's condition relative to their cardiac rhythm. It is different from hemodynamic monitoring, which monitors the pressure and flow of blood within the cardiovascular system. The two may be performed simultaneously on critical heart patients. Cardiac monitoring with a small device worn by an ambulatory patient is known as ambulatory electrocardiography. Transmitting data from a monitor to a distant monitoring station is known as telemetry or biotelemetry.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Coronary ischemia, myocardial ischemia, or cardiac ischemia, is a medical term for a reduced blood flow in the coronary circulation through the coronary arteries. Coronary ischemia is linked to heart disease, and heart attacks. Coronary arteries deliver oxygen-rich blood to the heart muscle. Reduced blood flow to the heart associated with coronary ischemia can result in inadequate oxygen supply to the heart muscle. When oxygen supply to the heart is unable to keep up with oxygen demand from the muscle, the result is the characteristic symptoms of coronary ischemia, the most common of which is chest pain. Chest pain due to coronary ischemia commonly radiates to the arm or neck. Certain individuals such as women, diabetics, and the elderly may present with more varied symptoms. If blood flow through the coronary arteries is stopped completely, cardiac muscle cells may die, known as a myocardial infarction, or heart attack.
Roemheld syndrome (RS), or gastrocardiac syndrome, or gastric cardiac syndrome or Roemheld-Techlenburg-Ceconi-Syndrome or gastric-cardia, was a medical syndrome first coined by Ludwig von Roemheld (1871–1938) describing a cluster of cardiovascular symptoms stimulated by gastrointestinal changes. Although it is currently considered an obsolete medical diagnosis, recent studies have described similar clinical presentations and highlighted potential underlying mechanisms.

Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath or chest pain. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.