An artificial cardiac pacemaker or artificial pacemaker, and sometimes just pacemaker—although the term is also used to refer to the body's natural cardiac pacemaker—is a medical device, nowadays always implanted, that generates electrical pulses delivered by electrodes to the chambers of the heart, either the upper atria or lower ventricles. Each pulse causes the targeted chambers to contract and pump blood, thus regulating the function of the electrical conduction system of the heart.

Cardioversion is a medical procedure by which an abnormally fast heart rate (tachycardia) or other cardiac arrhythmia is converted to a normal rhythm using electricity or drugs. Synchronized electrical cardioversion uses a therapeutic dose of electric current to the heart at a specific moment in the cardiac cycle, restoring the activity of the electrical conduction system of the heart. Pharmacologic cardioversion, also called chemical cardioversion, uses antiarrhythmia medication instead of an electrical shock.

Defibrillation is a treatment for life-threatening cardiac arrhythmias, specifically ventricular fibrillation (V-Fib) and non-perfusing ventricular tachycardia (V-Tach). A defibrillator delivers a dose of electric current to the heart. Although not fully understood, this process depolarizes a large amount of the heart muscle, ending the arrhythmia. Subsequently, the body's natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm. A heart which is in asystole (flatline) cannot be restarted by a defibrillator, but would be treated by cardiopulmonary resuscitation (CPR).

Ventricular fibrillation is an abnormal heart rhythm in which the ventricles of the heart quiver. It is due to disorganized electrical activity. Ventricular fibrillation results in cardiac arrest with loss of consciousness and no pulse. This is followed by sudden cardiac death in the absence of treatment. Ventricular fibrillation is initially found in about 10% of people with cardiac arrest.
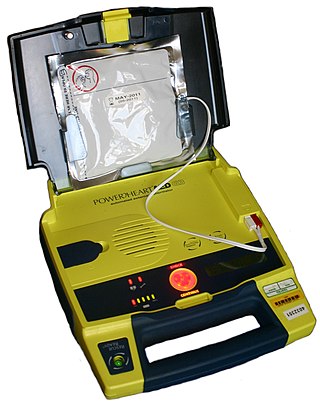
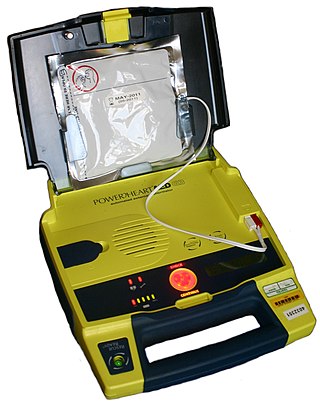
An automated external defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm.

An implantable cardioverter-defibrillator (ICD) or automated implantable cardioverter defibrillator (AICD) is a device implantable inside the body, able to perform defibrillation, and depending on the type, cardioversion and pacing of the heart. The ICD is the first-line treatment and prophylactic therapy for patients at risk for sudden cardiac death due to ventricular fibrillation and ventricular tachycardia.

Ventricular tachycardia is a fast heart rate arising from the lower chambers of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.
Precordial thump is a medical procedure used in the treatment of ventricular fibrillation or pulseless ventricular tachycardia under certain conditions. The procedure has a very low success rate, but may be used in those with witnessed, monitored onset of one of the "shockable" cardiac rhythms if a defibrillator is not immediately available. It should not delay cardiopulmonary resuscitation (CPR) and defibrillation, nor should it be used in those with unwitnessed out-of-hospital cardiac arrest.

Cardiac electrophysiology is a branch of cardiology and basic science focusing on the electrical activities of the heart. The term is usually used in clinical context, to describe studies of such phenomena by invasive (intracardiac) catheter recording of spontaneous activity as well as of cardiac responses to programmed electrical stimulation - clinical cardiac electrophysiology. However, cardiac electrophysiology also encompasses basic research and translational research components. Specialists studying cardiac electrophysiology, either clinically or solely through research, are known as cardiac electrophysiologists.
St. Jude Medical, Inc. was an American global medical device company headquartered in Little Canada, Minnesota, U.S., a suburb of Saint Paul. The company had more than 20 principal operations and manufacturing facilities worldwide with products sold in more than 100 countries. Its major markets include the United States, Europe, Latin America and Asia-Pacific. The company was named after Jude the Apostle, the patron saint of lost causes.
Clinical cardiac electrophysiology, is a branch of the medical specialty of cardiology and is concerned with the study and treatment of rhythm disorders of the heart. Cardiologists with expertise in this area are usually referred to as electrophysiologists. Electrophysiologists are trained in the mechanism, function, and performance of the electrical activities of the heart. Electrophysiologists work closely with other cardiologists and cardiac surgeons to assist or guide therapy for heart rhythm disturbances (arrhythmias). They are trained to perform interventional and surgical procedures to treat cardiac arrhythmia.

Transcutaneous pacing (TCP), also called external pacing, is a temporary means of pacing a patient's heart during a medical emergency. It should not be confused with defibrillation using a manual or automatic defibrillator, though some newer defibrillators can do both, and pads and an electrical stimulus to the heart are used in transcutaneous pacing and defibrillation. Transcutaneous pacing is accomplished by delivering pulses of electric current through the patient's chest, which stimulates the heart to contract.
Morton Maimon Mower was an American cardiologist specializing in electrophysiology and the co-inventor of the automatic implantable cardioverter defibrillator. He served in several professional capacities at Sinai Hospital and Cardiac Pacemakers Inc. In 1996, he became the chairman and chief executive officer of Mower Research Associates. He was inducted into the National Inventors Hall of Fame in 2002 for the development of the automatic implantable cardioverter defibrillator with Michel Mirowski in the 1970s. He continued his research in the biomechanical engineering laboratories at Johns Hopkins University.

Cardiac resynchronisation therapy is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ventricles via a pacemaker, a small device inserted into the anterior chest wall.
A wearable cardioverter defibrillator (WCD) is a non-invasive, external device for patients at risk of sudden cardiac arrest (SCA). It allows physicians time to assess their patient's arrhythmic risk and make appropriate plans. It is a leased device. A summary of the device, its technology and indications was published in 2017 and reviewed by the EHRA Scientific Documents Committee.
Boxer cardiomyopathy is a disease of the myocardium primarily affecting Boxer dogs. It is characterized by the development of ventricular tachyarrhythmias, resulting in syncope and sudden cardiac death. Myocardial failure and congestive heart failure are uncommon manifestations of the disease.
Cameron Health was a medical device developer based in San Clemente, California, USA. Cameron Health had its European office, Cameron Health BV, in Arnhem, The Netherlands. The privately held company's focus was on a new generation of minimally invasive implantable cardioverter-defibrillator (ICD) which they called a Subcutaneous Implantable Defibrillator (S-ICD). Cameron Health's approach avoided implanting transvenous leads into the heart, which had been the usual procedure for cardiac devices. Instead, the Cameron ICD was entirely implanted outside the thoracic wall.

Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath or chest pain. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.

Yaariv Khaykin is a Canadian cardiologist and a clinical researcher in the area of electrophysiology. He is the director of the Newmarket Electrophysiology Research Group at the Southlake Regional Health Centre. He has published research into complex ablation and pioneered cardiac ablation methods.
Defibrillation threshold indicates the minimum amount of energy needed to return normal rhythm to a heart that is beating in a cardiac dysrhythmia. Typical examples are the minimum amount of energy, expressed in joules, delivered by external defibrillator paddles or pads, required to break atrial fibrillation and restore normal sinus rhythm. Other common scenarios are restoring normal rhythm from atrial flutter, ventricular tachycardia or ventricular fibrillation. The defibrillation threshold ranking in these settings, from lowest to highest, would be, in order, ventricular tachycardia, atrial flutter, atrial fibrillation, ventricular fibrillation. The highest amount of energy that an external defibrillator can deliver at the present time is 360 joules biphasic. In clinical practice, the real threshold can be approximated but not exactly established, since the defibrillating shock can be delivered only once. Certain medications, in particular sotalol, tend to lower such threshold, while others, such as amiodarone, may increase it.