Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

Decompression sickness is a medical condition caused by dissolved gases emerging from solution as bubbles inside the body tissues during decompression. DCS most commonly occurs during or soon after a decompression ascent from underwater diving, but can also result from other causes of depressurisation, such as emerging from a caisson, decompression from saturation, flying in an unpressurised aircraft at high altitude, and extravehicular activity from spacecraft. DCS and arterial gas embolism are collectively referred to as decompression illness.
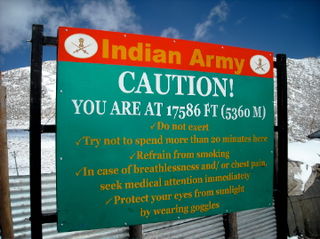
Altitude sickness, the mildest form being acute mountain sickness (AMS), is the harmful effect of high altitude, caused by rapid exposure to low amounts of oxygen at high elevation. People can respond to high altitude in different ways. Symptoms may include headaches, vomiting, tiredness, confusion, trouble sleeping, and dizziness. Acute mountain sickness can progress to high-altitude pulmonary edema (HAPE) with associated shortness of breath or high-altitude cerebral edema (HACE) with associated confusion. Chronic mountain sickness may occur after long-term exposure to high altitude.

Acetazolamide, sold under the trade name Diamox among others, is a medication used to treat glaucoma, epilepsy, altitude sickness, periodic paralysis, idiopathic intracranial hypertension, heart failure and to alkalinize urine. It may be used long term for the treatment of open angle glaucoma and short term for acute angle closure glaucoma until surgery can be carried out. It is taken by mouth or injection into a vein. Acetazolamide is a first generation carbonic anhydrase inhibitor and it decreases the ocular fluid and osmolality in the eye to decrease intraocular pressure.

The hematocrit, also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is normally 40.7–50.3% for males and 36.1–44.3% for females. It is a part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count and platelet count.
Hypoventilation occurs when ventilation is inadequate to perform needed respiratory gas exchange. By definition it causes an increased concentration of carbon dioxide (hypercapnia) and respiratory acidosis. Hypoventilation is not synonymous with respiratory arrest, in which breathing ceases entirely and death occurs within minutes due to hypoxia and leads rapidly into complete anoxia, although both are medical emergencies. Hypoventilation can be considered a precursor to hypoxia and its lethality is attributed to hypoxia with carbon dioxide toxicity.
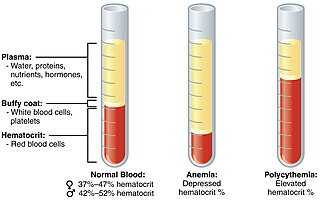
Polycythemia is a laboratory finding in which the hematocrit and/or hemoglobin concentration are increased in the blood. Polycythemia is sometimes called erythrocytosis, and there is significant overlap in the two findings, but the terms are not the same: polycythemia describes any increase in hematocrit and/or hemoglobin, while erythrocytosis describes an increase specifically in the number of red blood cells in the blood.
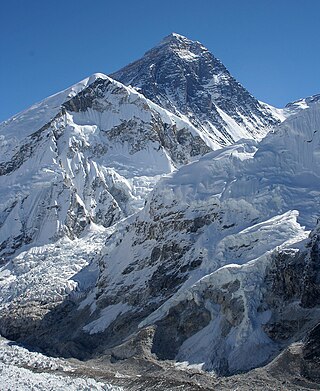
In mountaineering, the death zone refers to altitudes above a certain point where the pressure of oxygen is insufficient to sustain human life for an extended time span. This point is generally tagged as 8,000 m. The concept was conceived in 1953 by Edouard Wyss-Dunant, a Swiss doctor, who called it the lethal zone. All 14 peaks above 8000 m in the death zone are located in the Himalaya and Karakoram of Asia.

High-altitude pulmonary edema (HAPE) is a life-threatening form of non-cardiogenic pulmonary edema that occurs in otherwise healthy people at altitudes typically above 2,500 meters (8,200 ft). However, cases have also been reported between 1,500–2,500 metres or 4,900–8,200 feet in more vulnerable subjects.

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.
High-altitude cerebral edema (HACE) is a medical condition in which the brain swells with fluid because of the physiological effects of traveling to a high altitude. It generally appears in patients who have acute mountain sickness and involves disorientation, lethargy, and nausea among other symptoms. It occurs when the body fails to acclimatize while ascending to a high altitude.

2,3-Bisphosphoglyceric acid (2,3-BPG), also known as 2,3-diphosphoglyceric acid (2,3-DPG), is a three-carbon isomer of the glycolytic intermediate 1,3-bisphosphoglyceric acid (1,3-BPG).

Carbonic anhydrase inhibitors are a class of pharmaceuticals that suppress the activity of carbonic anhydrase. Their clinical use has been established as anti-glaucoma agents, diuretics, antiepileptics, in the management of mountain sickness, gastric and duodenal ulcers, idiopathic intracranial hypertension, neurological disorders, or osteoporosis.

The effects of high altitude on humans are mostly the consequences of reduced partial pressure of oxygen in the atmosphere. The oxygen saturation of hemoglobin determines the content of oxygen in blood. After the human body reaches around 2,100 metres (6,900 ft) above sea level, the saturation of oxyhemoglobin begins to decrease rapidly. However, the human body has both short-term and long-term adaptations to altitude that allow it to partially compensate for the lack of oxygen. There is a limit to the level of adaptation; mountaineers refer to the altitudes above 8,000 metres (26,000 ft) as the death zone, where it is generally believed that no human body can acclimatize. At extreme altitudes, the ambient pressure can drop below the vapor pressure of water at body temperature, but at such altitudes even pure oxygen at ambient pressure cannot support human life, and a pressure suit is necessary. A rapid depressurisation to the low pressures of high altitudes can trigger altitude decompression sickness.
Fabiola León-Velarde Servetto is a Peruvian physiologist who has devoted her research to the biology and physiology of high altitude adaptation. Born in Lima, Peru. She is the daughter of Carlos Leon-Velarde Gamarra and Juana Servetto Marti from Uruguay, and granddaughter of Angelica Gamarra. Under the mentorship of high altitude physiologist Carlos Monge Cassinelli, she obtained a BSc. in Biology (1979), an MSc (1981) and DSc (1986) in physiology at Cayetano Heredia University in Lima, Perú.
Endothelial PAS domain-containing protein 1 is a protein that is encoded by the EPAS1 gene in mammals. It is a type of hypoxia-inducible factor, a group of transcription factors involved in the physiological response to oxygen concentration. The gene is active under hypoxic conditions. It is also important in the development of the heart, and for maintaining the catecholamine balance required for protection of the heart. Mutation often leads to neuroendocrine tumors.
Hypoxic ventilatory response (HVR) is the increase in ventilation induced by hypoxia that allows the body to take in and transport lower concentrations of oxygen at higher rates. It is initially elevated in lowlanders who travel to high altitude, but reduces significantly over time as people acclimatize. In biological anthropology, HVR also refers to human adaptation to environmental stresses resulting from high altitude.

Organisms can live at high altitude, either on land, in water, or while flying. Decreased oxygen availability and decreased temperature make life at such altitudes challenging, though many species have been successfully adapted via considerable physiological changes. As opposed to short-term acclimatisation, high-altitude adaptation means irreversible, evolved physiological responses to high-altitude environments, associated with heritable behavioural and genetic changes. Among animals, only few mammals and certain birds are known to have completely adapted to high-altitude environments.
Gustavo Zubieta-Castillo was a Bolivian physician, high altitude medicine expert, physiologist, army surgeon, writer, painter, who was named as the "Mountain Guru" at the St. John's Medical College in Bangalore, India.
High-altitude adaptation in humans is an instance of evolutionary modification in certain human populations, including those of Tibet in Asia, the Andes of the Americas, and Ethiopia in Africa, who have acquired the ability to survive at altitudes above 2,500 meters. This adaptation means irreversible, long-term physiological responses to high-altitude environments, associated with heritable behavioural and genetic changes. While the rest of the human population would suffer serious health consequences, the indigenous inhabitants of these regions thrive well in the highest parts of the world. These humans have undergone extensive physiological and genetic changes, particularly in the regulatory systems of oxygen respiration and blood circulation, when compared to the general lowland population.
References
- 1 2 3 4 5 León-Velarde, F; Maggiorini, M; Reeves, JT; Aldashev, A; Asmus, I; et al. (2005). "Consensus statement on chronic and subacute high altitude diseases". High Altitude Medicine & Biology. 6 (2): 147–57. doi:10.1089/ham.2005.6.147. PMID 16060849.
- ↑ Wu, TY (20 January 2005). "Chronic mountain sickness on the Qinghai-Tibetan plateau". Chinese Medical Journal. 118 (2): 161–8. PMID 15667803.
- ↑ Monge, CC; Whittembury, J (December 1976). "Chronic mountain sickness". The Johns Hopkins Medical Journal. 139 SUPPL: 87–9. PMID 1011412.
- ↑ Zhou, D; Udpa, N; Ronen, R; Stobdan, T; Liang, J; et al. (5 September 2013). "Whole-genome sequencing uncovers the genetic basis of chronic mountain sickness in Andean highlanders". American Journal of Human Genetics. 93 (3): 452–62. doi:10.1016/j.ajhg.2013.07.011. PMC 3769925 . PMID 23954164.
- ↑ Cole, AM; Petousi, N; Cavalleri, GL; Robbins, PA (December 2014). "Genetic variation in SENP1 and ANP32D as predictors of chronic mountain sickness". High Altitude Medicine & Biology. 15 (4): 497–9. doi:10.1089/ham.2014.1036. PMC 4273201 . PMID 25225945.
- ↑ Zubieta-Castillo G, Sr; Zubieta-Calleja GR, Jr; Zubieta-Calleja, L (September 2006). "Chronic mountain sickness: the reaction of physical disorders to chronic hypoxia". Journal of Physiology and Pharmacology. 57 Suppl 4: 431–42. PMID 17072074.
- ↑ Richalet, JP; Rivera, M; Bouchet, P; Chirinos, E; Onnen, I; et al. (1 December 2005). "Acetazolamide: a treatment for chronic mountain sickness". American Journal of Respiratory and Critical Care Medicine. 172 (11): 1427–33. doi:10.1164/rccm.200505-807OC. PMID 16126936.
- ↑ Sahota, I; Panwar, N (September 2013). "Prevalence of Chronic Mountain Sickness in high altitude districts of Himachal Pradesh". Indian Journal of Occupational and Environmental Medicine. 17 (3): 94–100. doi:10.4103/0019-5278.130839. PMC 4035612 . PMID 24872667.