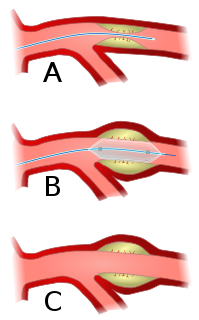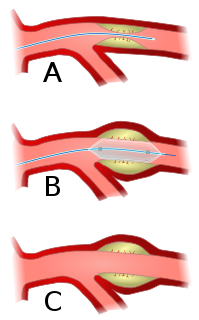
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.

Deep vein thrombosis (DVT) is the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms. The most common life-threatening concern with DVT is the potential for a clot to embolize, travel as an embolus through the right side of the heart, and become lodged in a pulmonary artery that supplies blood to the lungs. This is called a pulmonary embolism (PE). DVT and PE comprise the cardiovascular disease of venous thromboembolism (VTE). About two-thirds of VTE manifests as DVT only, with one-third manifesting as PE with or without DVT. The most frequent long-term DVT complication is post-thrombotic syndrome, which can cause pain, swelling, a sensation of heaviness, itching, and in severe cases, ulcers. Recurrent VTE occurs in about 30% of those in the ten years following an initial VTE.

A coronary catheterization is a minimally invasive procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It is performed for both diagnostic and interventional (treatment) purposes.

dextro-Transposition of the great arteries, is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.

Mitral stenosis is a valvular heart disease characterized by the narrowing of the orifice of the mitral valve of the heart. It is almost always caused by rheumatic valvular heart disease. Normally, the mitral valve is about 5 cm2 during diastole. Any decrease in area below 2 cm2 causes mitral stenosis. Early diagnosis of mitral stenosis in pregnancy is very important as the heart cannot tolerate increased cardiac output demand as in the case of exercise and pregnancy. Atrial fibrillation is a common complication of resulting left atrial enlargement, which can lead to systemic thromboembolic complications like stroke.
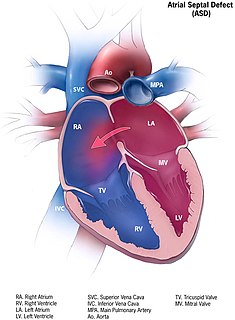
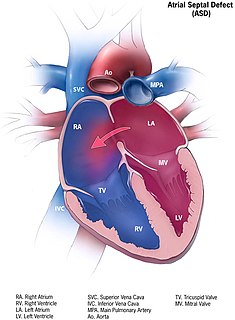
Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this does not naturally close after birth it is referred to as a patent (open) foramen ovale (PFO). It is common in patients with a congenital atrial septal aneurysm (ASA).

Portal hypertension is abnormally increased portal venous pressure – blood pressure in the portal vein and its branches, that drain from most of the intestine to the liver. Portal hypertension is defined as a hepatic venous pressure gradient greater than 5 mmHg. Cirrhosis is the most common cause of portal hypertension; other, less frequent causes are therefore grouped as non-cirrhotic portal hypertension. When it becomes severe enough to cause symptoms or complications, treatment may be given to decrease portal hypertension itself or to manage its complications.
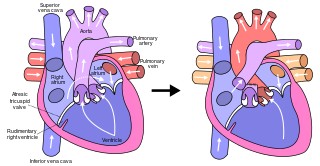
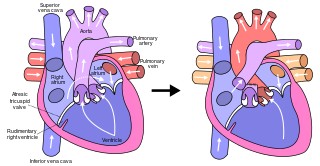
The Fontan procedure or Fontan–Kreutzer procedure is a palliative surgical procedure used in children with univentricular hearts. It involves diverting the venous blood from the inferior vena cava (IVC) and superior vena cava (SVC) to the pulmonary arteries without passing through the morphologic right ventricle; i.e., the systemic and pulmonary circulations are placed in series with the functional single ventricle. The procedure was initially performed in 1968 by Francis Fontan and Eugene Baudet from Bordeaux, France, published in 1971, simultaneously described in 1971 by Guillermo Kreutzer from Buenos Aires, Argentina, and finally published in 1973.

Coarctation of the aorta, also called aortic narrowing, is a congenital condition whereby the aorta is narrow, usually in the area where the ductus arteriosus inserts. The word coarctation means "pressing or drawing together; narrowing". Coarctations are most common in the aortic arch. The arch may be small in babies with coarctations. Other heart defects may also occur when coarctation is present, typically occurring on the left side of the heart. When a patient has a coarctation, the left ventricle has to work harder. Since the aorta is narrowed, the left ventricle must generate a much higher pressure than normal in order to force enough blood through the aorta to deliver blood to the lower part of the body. If the narrowing is severe enough, the left ventricle may not be strong enough to push blood through the coarctation, thus resulting in a lack of blood to the lower half of the body. Physiologically its complete form is manifested as interrupted aortic arch.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.
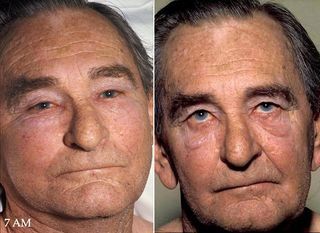
Superior vena cava syndrome (SVCS), is a group of symptoms caused by obstruction of the superior vena cava ("SVC"), a short, wide vessel carrying circulating blood into the heart. The majority of cases are caused by malignant tumors within the mediastinum, most commonly lung cancer and non-Hodgkin's lymphoma, directly compressing or invading the SVC wall. Non-malignant causes are increasing in prevalence due to expanding use of intravascular devices, which can result in thrombosis. Other non-malignant causes include benign mediastinal tumors, aortic aneurysm, infections, and fibrosing mediastinitis.
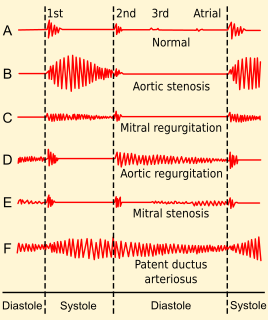
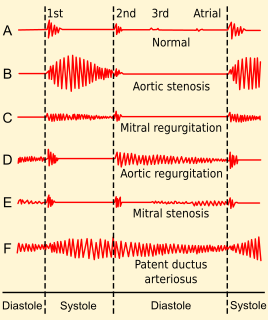
Valvular heart disease is any cardiovascular disease process involving one or more of the four valves of the heart. These conditions occur largely as a consequence of aging, but may also be the result of congenital (inborn) abnormalities or specific disease or physiologic processes including rheumatic heart disease and pregnancy.

Inferior vena cava syndrome (IVCS) is a constellation of symptoms resulting from obstruction of the inferior vena cava. It can be caused by physical invasion or compression by a pathological process or by thrombosis within the vein itself. It can also occur during pregnancy. Pregnancy leads to high venous pressure in the lower limbs, decreased blood return to the heart, decreased cardiac output due to obstruction of the inferior vena cava, sudden rise in venous pressure which can lead to placental separation, and a decrease in kidney function. All of these issues can arise from lying in the supine position during late pregnancy which can cause compression of the inferior vena cava by the uterus. Symptoms of late pregnancy inferior vena cava syndrome consist of intense pain in the right hand side, muscle twitching, hypotension, and fluid retention.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).

Pulmonary valve stenosis (PVS) is a heart valve disorder. Blood going from the heart to the lungs goes through the pulmonary valve, whose purpose is to prevent blood from flowing back to the heart. In pulmonary valve stenosis this opening is too narrow, leading to a reduction of flow of blood to the lungs.

May–Thurner syndrome (MTS), also known as the iliac vein compression syndrome, is a condition in which compression of the common venous outflow tract of the left lower extremity may cause discomfort, swelling, pain or clots in the iliofemoral veins.

Venography is a procedure in which an x-ray of the veins, a venogram, is taken after a special dye is injected into the bone marrow or veins. The dye has to be injected constantly via a catheter, making it an invasive procedure. Normally the catheter is inserted by the groin and moved to the appropriate site by navigating through the vascular system.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein. The most common cause of CVI is superficial venous reflux which is a treatable condition. As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.

Anomalous pulmonary venous connection is a congenital defect of the pulmonary veins.