Leukotrienes are a family of eicosanoid inflammatory mediators produced in leukocytes by the oxidation of arachidonic acid (AA) and the essential fatty acid eicosapentaenoic acid (EPA) by the enzyme arachidonate 5-lipoxygenase.

Zafirlukast is an orally administered leukotriene receptor antagonist (LTRA) used for the chronic treatment of asthma. While zafirlukast is generally well tolerated, headache and stomach upset often occur. Some rare side effects can occur, which can be life-threatening, such as liver failure. Churg-Strauss syndrome has been associated with zafirlukast, but the relationship isn't thought to be causative in nature. Overdoses of zafirlukast tend to be self-limiting.

Montelukast, sold under the brand name Singulair among others, is a medication used in the maintenance treatment of asthma. It is generally less preferred for this use than inhaled corticosteroids. It is not useful for acute asthma attacks. Other uses include allergic rhinitis and hives of long duration. For allergic rhinitis it is a second-line treatment.

Aspirin exacerbated respiratory disease (AERD), also termed aspirin-induced asthma, is a medical condition initially defined as consisting of three key features: asthma, respiratory symptoms exacerbated by aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), and nasal polyps. The symptoms of respiratory reactions in this syndrome are hypersensitivity reactions to NSAIDs rather than the typically described true allergic reactions that trigger other common allergen-induced asthma, rhinitis, or hives. The NSAID-induced reactions do not appear to involve the common mediators of true allergic reactions, immunoglobulin E or T cells. Rather, AERD is a type of NSAID-induced hypersensitivity syndrome. EAACI/WHO classifies the syndrome as one of five types of NSAID hypersensitivity or NSAID hypersensitivity reactions.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

Ketotifen, sold under the brand name Zaditor among others, is a second-generation noncompetitive H1-antihistamine and mast cell stabilizer. It is most commonly sold as a salt with fumaric acid, ketotifen fumarate, and is available in two forms. In its ophthalmic form, it is used to treat allergic conjunctivitis. In its oral form, it is used to prevent asthma attacks or anaphylaxis, as well as various mast cell, allergic-type disorders.

Pranlukast is a cysteinyl leukotriene receptor-1 antagonist. This drug works similarly to Merck & Co.'s montelukast (Singulair). It is widely used in Japan.

The thromboxane receptor (TP) also known as the prostanoid TP receptor is a protein that in humans is encoded by the TBXA2R gene, The thromboxane receptor is one among the five classes of prostanoid receptors and was the first eicosanoid receptor cloned. The TP receptor derives its name from its preferred endogenous ligand thromboxane A2.
An antileukotriene, also known as leukotriene modifier and leukotriene receptor antagonist, is a medication which functions as a leukotriene-related enzyme inhibitor or leukotriene receptor antagonist and consequently opposes the function of these inflammatory mediators; leukotrienes are produced by the immune system and serve to promote bronchoconstriction, inflammation, microvascular permeability, and mucus secretion in asthma and COPD. Leukotriene receptor antagonists are sometimes colloquially referred to as leukasts.

Leukotriene E4 (LTE4) is a cysteinyl leukotriene involved in inflammation. It is known to be produced by several types of white blood cells, including eosinophils, mast cells, tissue macrophages, and basophils, and recently was also found to be produced by platelets adhering to neutrophils. It is formed from the sequential conversion of LTC4 to LTD4 and then to LTE4, which is the final and most stable cysteinyl leukotriene. Compared to the short half lives of LTC4 and LTD4, LTE4 is relatively stable and accumulates in breath condensation, in plasma, and in urine, making it the dominant cysteinyl leukotriene detected in biologic fluids. Therefore, measurements of LTE4, especially in the urine, are commonly monitored in clinical research studies.
Most of the eicosanoid receptors are integral membrane protein G protein-coupled receptors (GPCRs) that bind and respond to eicosanoid signaling molecules. Eicosanoids are rapidly metabolized to inactive products and therefore are short-lived. Accordingly, the eicosanoid-receptor interaction is typically limited to a local interaction: cells, upon stimulation, metabolize arachidonic acid to an eicosanoid which then binds cognate receptors on either its parent cell or on nearby cells to trigger functional responses within a restricted tissue area, e.g. an inflammatory response to an invading pathogen. In some cases, however, the synthesized eicosanoid travels through the blood to trigger systemic or coordinated tissue responses, e.g. prostaglandin (PG) E2 released locally travels to the hypothalamus to trigger a febrile reaction. An example of a non-GPCR receptor that binds many eicosanoids is the PPAR-γ nuclear receptor.

Leukotriene D4 (LTD4) is one of the leukotrienes. Its main function in the body is to induce the contraction of smooth muscle, resulting in bronchoconstriction and vasoconstriction. It also increases vascular permeability. LTD4 is released by basophils. Other leukotrienes that function in a similar manner are leukotrienes C4 and E4. Pharmacological agents that inhibit the function of these leukotrienes are leukotriene receptor antagonists (e.g., zafirlukast, montelukast) and are useful for asthmatic individuals.

Uracil nucleotide/cysteinyl leukotriene receptor is a G protein-coupled receptor that in humans is encoded by the GPR17 gene located on chromosome 2 at position q21. The actual activating ligands for and some functions of this receptor are disputed.

Cysteinyl leukotriene receptor 1, also termed CYSLTR1, is a receptor for cysteinyl leukotrienes (LT). CYSLTR1, by binding these cysteinyl LTs contributes to mediating various allergic and hypersensitivity reactions in humans as well as models of the reactions in other animals.

2-Oxoglutarate receptor 1 (OXGR1), also known as cysteinyl leukotriene receptor E (CysLTE) and GPR99, is a protein that in humans is encoded by the OXGR1 gene. The Gene has recently been nominated as a receptor not only for 2-oxogluterate but also for the three cysteinyl leukotrienes (CysLTs), particularly leukotriene E4 (LTE4) and to far lesser extents LTC4 and LTE4. Recent studies implicate GPR99 as a cellular receptor which is activated by LTE4 thereby causing these cells to contribute to mediating various allergic and hypersensitivity responses.

Cysteinyl leukotriene receptor 2, also termed CYSLTR2, is a receptor for cysteinyl leukotrienes (LT). CYSLTR2, by binding these cysteinyl LTs contributes to mediating various allergic and hypersensitivity reactions in humans. However, the first discovered receptor for these CsLTs, cysteinyl leukotriene receptor 1 (CysLTR1), appears to play the major role in mediating these reactions.
A cannabinoid receptor antagonist, also known simply as a cannabinoid antagonist or as an anticannabinoid, is a type of cannabinoidergic drug that binds to cannabinoid receptors (CBR) and prevents their activation by endocannabinoids. They include antagonists, inverse agonists, and antibodies of CBRs. The discovery of the endocannabinoid system led to the development of CB1 receptor antagonists. The first CBR inverse agonist, rimonabant, was described in 1994. Rimonabant blocks the CB1 receptor selectively and has been shown to decrease food intake and regulate body-weight gain. The prevalence of obesity worldwide is increasing dramatically and has a great impact on public health. The lack of efficient and well-tolerated drugs to cure obesity has led to an increased interest in research and development of CBR antagonists. Cannabidiol (CBD), a naturally occurring cannabinoid, is a non-competitive CB1/CB2 receptor antagonist. And Δ9-tetrahydrocannabivarin (THCV), a naturally occurring cannabinoid, modulate the effects of THC via direct blockade of cannabinoid CB1 receptors, thus behaving like first-generation CB1 receptor inverse agonists, such as rimonabant. CBD is a very low-affinity CB1 ligand, that can nevertheless affect CB1 receptor activity in vivo in an indirect manner, while THCV is a high-affinity CB1 receptor ligand and potent antagonist in vitro and yet only occasionally produces effects in vivo resulting from CB1 receptor antagonism. THCV has also high affinity for CB2 receptors and signals as a partial agonist, differing from both CBD and rimonabant.
Relief from chronic pain remains a recognized unmet medical need. Consequently, the search for new analgesic agents is being intensively studied by the pharmaceutical industry. The TRPV1 receptor is an ion channel that has been implicated in mediation of many types of pain and therefore studied most extensively. The first competitive antagonist, capsazepine, was first described in 1990, since then development of novel TRPV1 antagonists has come a long way. This effort has led to the identification of several TRPV1 antagonists that have entered clinical trials as analgesic agents. Should these new chemical entities relieve symptoms of chronic pain then this class of compounds may offer one of the first novel mechanisms for the treatment of pain, in many years.
The leukotriene (LT) receptors are G protein-coupled receptors that bind and are activated by the leukotrienes. They include the following proteins:
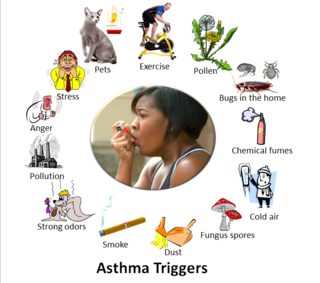
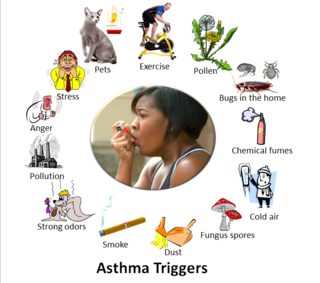
Asthma triggers are factors or stimuli that provoke the exacerbation of asthma symptoms or increase the degree of airflow disruption, which can lead to an asthma attack. An asthma attack is characterized by an obstruction of the airway, hypersecretion of mucus and bronchoconstriction due to the contraction of smooth muscles around the respiratory tract. Its symptoms include a wide range of manifestations such as breathlessness, coughing, a tight chest and wheezing.