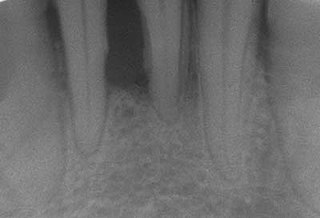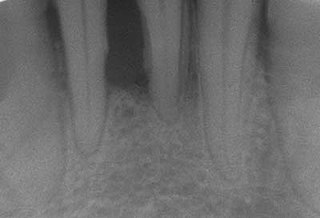
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen, red, and may bleed. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or fall out. Bad breath may also occur.

A dentist, also known as a dental surgeon, is a surgeon who specializes in dentistry, the diagnosis, prevention, and treatment of diseases and conditions of the oral cavity. The dentist's supporting team aids in providing oral health services. The dental team includes dental assistants, dental hygienists, dental technicians, and sometimes dental therapists.

Cementum is a specialized calcified substance covering the root of a tooth. The cementum is the part of the periodontium that attaches the teeth to the alveolar bone by anchoring the periodontal ligament.

The gums or gingiva, consist of the mucosal tissue that lies over the mandible and maxilla inside the mouth. Gum health and disease can have an effect on general health.

Dental alveoli are sockets in the jaws in which the roots of teeth are held in the alveolar process with the periodontal ligament. The lay term for dental alveoli is tooth sockets. A joint that connects the roots of the teeth and the alveolus is called gomphosis. Alveolar bone is the bone that surrounds the roots of the teeth forming bone sockets.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.

Gingival recession, also known as receding gums, is the exposure in the roots of the teeth caused by a loss of gum tissue and/or retraction of the gingival margin from the crown of the teeth. Gum recession is a common problem in adults over the age of 40, but it may also occur starting from the age of a teenager, or around the age of 10. It may exist with or without concomitant decrease in crown-to-root ratio.

Crown lengthening is a surgical procedure performed by a dentist, or more frequently a specialist periodontist. There are a number of reasons for considering crown lengthening in a treatment plan. Commonly, the procedure is used to expose a greater amount of tooth structure for the purpose of subsequently restoring the tooth prosthetically. However, other indications include accessing subgingival caries, accessing perforations and to treat aesthetic disproportions such as a gummy smile. There are a number of procedures used to achieve an increase in crown length.

Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy, or deep cleaning, is a procedure involving removal of dental plaque and calculus and then smoothing, or planing, of the (exposed) surfaces of the roots, removing cementum or dentine that is impregnated with calculus, toxins, or microorganisms, the etiologic agents that cause inflammation. This helps to establish a periodontium that is in remission of periodontal disease. Periodontal scalers and periodontal curettes are some of the tools involved.

In dentistry, the subepithelial connective tissue graft is an oral and maxillofacial surgical procedure first described by Alan Edel in 1974. Currently, it is generally used to obtain root coverage following gingival recession, which was a later development by Burt Langer in the early 1980s.
Guided bone regeneration (GBR) and guided tissue regeneration (GTR) are dental surgical procedures that use barrier membranes to direct the growth of new bone and gingival tissue at sites with insufficient volumes or dimensions of bone or gingiva for proper function, esthetics or prosthetic restoration. Guided bone regeneration typically refers to ridge augmentation or bone regenerative procedures; guided tissue regeneration typically refers to regeneration of periodontal attachment.
W. J. Younger (1838-1920) was an American dentist who performed some of the earliest and most groundbreaking research in the field of periodontology.
A barrier membrane is a device used in oral surgery and periodontal surgery to prevent epithelium, which regenerates relatively quickly, from growing into an area in which another, more slowly growing tissue type, such as bone, is desired. Such a method of preventing epithelial migration into a specific area is known as guided tissue regeneration (GTR).
Acellular dermis is a type of biomaterial derived from processing human or animal tissues to remove cells and retain portions of the extracellular matrix (ECM). These materials are typically cell-free, distinguishing them from classical allografts and xenografts, can be integrated or incorporated into the body, and have been FDA approved for human use for more than 10 years in a wide range of clinical indications.

Chronic periodontitis is a common disease of the oral cavity consisting of chronic inflammation of the periodontal tissues that is caused by the accumulation of profuse amounts of dental plaque. Periodontitis initially begins as gingivitis and can progress onto chronic and subsequent aggressive periodontitis according to the 1999 classification. Diagnosing chronic periodontitis is important in its early stages to prevent severe and irreversable damage to the protective and supportive structures of the tooth. However, due to chronic periodontitis being a painless progressing disease, few patients will seek dental care in the early stages. Mild to moderate chronic periodontitis can be managed by proper mechanical removal of the biofilm and calculus subgingivally. Full and effective oral hygiene and regular 3 monthly periodontal checkups are important for maintaining the stability of the disease.
Tissue engineering of oral mucosa combines cells, materials and engineering to produce a three-dimensional reconstruction of oral mucosa. It is meant to simulate the real anatomical structure and function of oral mucosa. Tissue engineered oral mucosa shows promise for clinical use, such as the replacement of soft tissue defects in the oral cavity. These defects can be divided into two major categories: the gingival recessions which are tooth-related defects, and the non tooth-related defects. Non tooth-related defects can be the result of trauma, chronic infection or defects caused by tumor resection or ablation. Common approaches for replacing damaged oral mucosa are the use of autologous grafts and cultured epithelial sheets.

Angularis nigra, Latin for 'black angle', also known as open gingival embrasures, and colloquially known as "black triangle", is the space or gap seen at the cervical embrasure, below the contact point of some teeth. The interdental papilla does not fully enclose the space, leading to an aperture between adjacent teeth. This gap has many causes including gingival recession, and gingival withdrawal post-orthodontic work. Interdental "black triangles" were rated as the third-most-disliked aesthetic problem below caries and crown margins. Treatment of angularis nigra often requires an interdisciplinary approach, involving periodontal, orthodontic and restorative treatment. Possible treatments to correct angularis nigra include addition of composite resin in the space, veneer placement, or gum graft. Angularis nigra is generally only treated based on the aesthetic preference of the patient.
Hereditary gingival fibromatosis (HGF), also known as idiopathic gingival hyperplasia, is a rare condition of gingival overgrowth. HGF is characterized as a benign, slowly progressive, nonhemorrhagic, fibrous enlargement of keratinized gingiva. It can cover teeth in various degrees, and can lead to aesthetic disfigurement. Fibrous enlargement is most common in areas of maxillary and mandibular tissues of both arches in the mouth. Phenotype and genotype frequency of HGF is 1:175,000 where males and females are equally affected but the cause is not entirely known. It mainly exists as an isolated abnormality but can also be associated with a multi-system syndrome.
Platelet-rich fibrin (PRF) or leukocyte- and platelet-rich fibrin (L-PRF) is a second-generation PRP where autologous platelets and leukocytes are present in a complex fibrin matrix to accelerate the healing of soft and hard tissue and is used as a tissue-engineering scaffold for endodontics. To obtain PRF, required quantity of blood is drawn quickly into test tubes without an anticoagulant and centrifuged immediately. Blood can be centrifuged using a tabletop centrifuge for at least 10 min at 3000 revolution per minute. The resultant product consists of the following three layers; topmost layer consisting of platelet poor plasma, PRF clot in the middle, and red blood cells (RBC) at the bottom. PRF is available as a fibrin clot. PRF clot can be removed from the test tube using a sterile tweezer-like instrument. After lifting, the RBC layer attached to the PRF clot can be carefully removed using a sterilized scissor. Platelet activation in response to tissue damage occurs during the process of making PRF release several biologically active proteins including; platelet alpha granules, platelet‑derived growth factor (PGDF), transforming growth factors‑β (TGF‑β), vascular endothelial growth factor (VEGF), and epidermal growth factor. Actually, the platelets and leukocyte cytokines play important parts in role of this biomaterial, but the fibrin matrix supporting them is the most helpful in constituting the determining elements responsible for real therapeutic potential of PRF. Cytokines are immediately used and destroyed in a healing wound. The harmony between cytokines and their supporting fibrin matrix has much more importance than any other platelet derivatives.
Hector L. Sarmiento is an American periodontist involved in dental implant complications research.