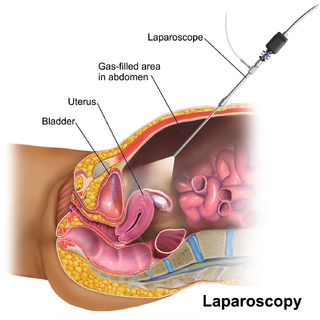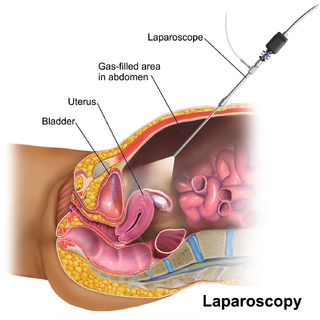
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.
Asplenia refers to the absence of normal spleen function and is associated with some serious infection risks. Hyposplenism is used to describe reduced ('hypo-') splenic functioning, but not as severely affected as with asplenism.

Influenza vaccines, colloquially known as flu shots or the flu jab, are vaccines that protect against infection by influenza viruses. New versions of the vaccines are developed twice a year, as the influenza virus rapidly changes. While their effectiveness varies from year to year, most provide modest to high protection against influenza. Vaccination against influenza began in the 1930s, with large-scale availability in the United States beginning in 1945.

On December 31, 2019, China announced the discovery of a cluster of pneumonia cases in Wuhan. The first American case was reported on January 20, and Health and Human Services Secretary Alex Azar declared a public health emergency on January 31. Restrictions were placed on flights arriving from China, but the initial U.S. response to the pandemic was otherwise slow in terms of preparing the healthcare system, stopping other travel, and testing. The first known American deaths occurred in February and in late February President Donald Trump proposed allocating $2.5 billion to fight the outbreak. Instead, Congress approved $8.3 billion with only Senator Rand Paul and two House representatives voting against, and Trump signed the bill, the Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, on March 6. Trump declared a national emergency on March 13. The government also purchased large quantities of medical equipment, invoking the Defense Production Act of 1950 to assist. By mid-April, disaster declarations were made by all states and territories as they all had increasing cases. A second wave of infections began in June, following relaxed restrictions in several states, leading to daily cases surpassing 60,000. By mid-October, a third surge of cases began; there were over 200,000 new daily cases during parts of December 2020 and January 2021.
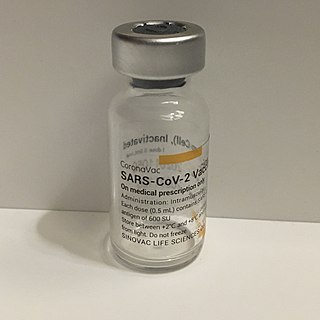
A COVID‑19 vaccine is a vaccine intended to provide acquired immunity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID‑19).

The COVID-19 pandemic has impacted hospitals around the world. Many hospitals have scaled back or postponed non-emergency care. This has medical consequences for the people served by the hospitals, and it has financial consequences for the hospitals. Health and social systems across the globe are struggling to cope. The situation is especially challenging in humanitarian, fragile and low-income country contexts, where health and social systems are already weak. Health facilities in many places are closing or limiting services. Services to provide sexual and reproductive health care risk being sidelined, which will lead to higher maternal mortality and morbidity. The pandemic also resulted in the imposition of COVID-19 vaccine mandates in places such as California and New York for all public workers, including hospital staff.

The Oxford–AstraZeneca COVID‑19 vaccine, sold under the brand names Covishield and Vaxzevria among others, is a viral vector vaccine for the prevention of COVID-19. It was developed in the United Kingdom by Oxford University and British-Swedish company AstraZeneca, using as a vector the modified chimpanzee adenovirus ChAdOx1. The vaccine is given by intramuscular injection. Studies carried out in 2020 showed that the efficacy of the vaccine is 76.0% at preventing symptomatic COVID-19 beginning at 22 days following the first dose and 81.3% after the second dose. A study in Scotland found that, for symptomatic COVID-19 infection after the second dose, the vaccine is 81% effective against the Alpha variant and 61% against the Delta variant.
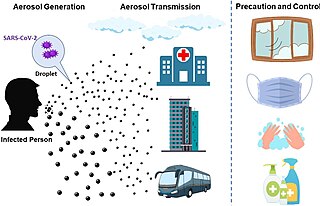
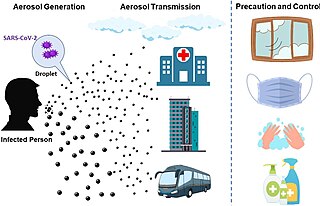
The transmission of COVID-19 is the passing of coronavirus disease 2019 from person to person. COVID-19 is mainly transmitted when people breathe in air contaminated by droplets/aerosols and small airborne particles containing the virus. Infected people exhale those particles as they breathe, talk, cough, sneeze, or sing. Transmission is more likely the closer people are. However, infection can occur over longer distances, particularly indoors.
Azeem Majeed is a Professor and Head of the Department of Primary Care & Public Health at Imperial College, London, as well as a general practitioner in South London and a consultant in public health. In the most recent UK University Research Excellence Framework results, Imperial College London was the highest ranked university in the UK for the quality of research in the “Public Health, Health Services and Primary Care” unit of assessment.

Vaccine diplomacy, a form of medical diplomacy, is the use of vaccines to improve a country's diplomatic relationship and influence of other countries. Meanwhile, vaccine diplomacy also "means a set of diplomatic measures taken to ensure access to the best practices in the development of potential vaccines, to enhance bilateral and/or multilateral cooperation between countries in conducting joint R&D, and, in the case of the announcement of production, to ensure the signing of a contract for the purchase of the vaccine at the shortest term." Although primary discussed in the context of the supply of COVID-19 vaccines, it also played a part in the distribution of the smallpox vaccine.
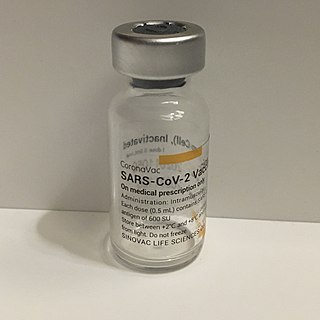
CoronaVac, also known as the Sinovac COVID-19 vaccine, was a whole inactivated virus COVID-19 vaccine developed by the Chinese company Sinovac Biotech. It was phase III clinically trialled in Brazil, Chile, Indonesia, the Philippines, and Turkey and relies on traditional technology similar to other inactivated-virus COVID-19 vaccines, such as the Sinopharm BIBP vaccine, another Chinese vaccine, and Covaxin, an Indian vaccine. CoronaVac does not need to be frozen, and both the final product and the raw material for formulating CoronaVac can be transported refrigerated at 2–8 °C (36–46 °F), the temperatures at which flu vaccines are kept.

The Pfizer–BioNTech COVID-19 vaccine, sold under the brand name Comirnaty, is an mRNA-based COVID-19 vaccine developed by the German biotechnology company BioNTech. For its development, BioNTech collaborated with the American company Pfizer to carry out clinical trials, logistics, and manufacturing. It is authorized for use in humans to provide protection against COVID-19, caused by infection with the SARS-CoV-2 virus. The vaccine is given by intramuscular injection. It is composed of nucleoside-modified mRNA (modRNA) that encodes a mutated form of the full-length spike protein of SARS-CoV-2, which is encapsulated in lipid nanoparticles. Initial guidance recommended a two-dose regimen, given 21 days apart; this interval was subsequently extended to up to 42 days in the United States, and up to four months in Canada.

The COVID-19 vaccination programme in the United Kingdom is an ongoing mass immunisation campaign for coronavirus disease 2019 (COVID-19) during the COVID-19 pandemic in the United Kingdom.

Israel's COVID-19 vaccination programme, officially named "Give a Shoulder", began on 19 December 2020, and has been praised for its speed, having given twenty percent of the Israeli population the first dose of the vaccines' two dose regimen in the span of three weeks.

As of 12 August 2024, 13.53 billion COVID-19 vaccine doses have been administered worldwide, with 70.6 percent of the global population having received at least one dose. While 4.19 million vaccines were then being administered daily, only 22.3 percent of people in low-income countries had received at least a first vaccine by September 2022, according to official reports from national health agencies, which are collated by Our World in Data.

Martin Kulldorff is a Swedish biostatistician. He was a professor of medicine at Harvard Medical School from 2003 until his dismissal in 2024. He is a member of the US Food and Drug Administration's Drug Safety and Risk Management Advisory Committee and a former member of the Vaccine Safety Subgroup of the Advisory Committee on Immunization Practices at the Centers for Disease Control and Prevention.

The COVID-19 vaccination programme in the Republic of Ireland is an ongoing mass immunisation campaign that began on 29 December 2020 in response to the COVID-19 pandemic in the Republic of Ireland. Ireland's vaccination rollout has been praised as one of the most successful rollouts in the world and was ranked number one in the European Union in terms of its percentage of adult population fully vaccinated, and was also ranked number one in the EU for the number of booster vaccines administered.
Peter Andrew McCullough is an American cardiologist. He was vice chief of internal medicine at Baylor University Medical Center and a professor at Texas A&M University. From the beginnings of the COVID-19 pandemic, McCullough has promoted misinformation about COVID-19, its treatments, and mRNA vaccines.
Fractional dose vaccination is a strategy to reduce the dose of a vaccine to achieve a vaccination policy goal that is more difficult to achieve with conventional vaccination approaches, including deploying a vaccine faster in a pandemic, reaching more individuals in the setting of limited healthcare budgets, or minimizing side effects due to the vaccine.

In many countries a variety of unfounded conspiracy theories and other misinformation about COVID-19 vaccines have spread based on misunderstood or misrepresented science, religion, and law. These have included exaggerated claims about side effects, misrepresentations about how the immune system works and when and how COVID-19 vaccines are made, a story about COVID-19 being spread by 5G, and other false or distorted information. This misinformation, some created by anti-vaccination activists, has proliferated and may have made many people averse to vaccination. This has led to governments and private organizations around the world introducing measures to incentivize or coerce vaccination, such as lotteries, mandates, and free entry to events, which has in turn led to further misinformation about the legality and effect of these measures themselves.