Related Research Articles

Acute disseminated encephalomyelitis (ADEM), or acute demyelinating encephalomyelitis, is a rare autoimmune disease marked by a sudden, widespread attack of inflammation in the brain and spinal cord. As well as causing the brain and spinal cord to become inflamed, ADEM also attacks the nerves of the central nervous system and damages their myelin insulation, which, as a result, destroys the white matter. The cause is often a trigger such as from viral infection or vaccinations.
Multiplesclerosis (MS) is the most common demyelinating disease, in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This damage disrupts the ability of parts of the nervous system to transmit signals, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Specific symptoms can include double vision, visual loss, muscle weakness, and trouble with sensation or coordination. MS takes several forms, with new symptoms either occurring in isolated attacks or building up over time. In the relapsing forms of MS, between attacks, symptoms may disappear completely, although some permanent neurological problems often remain, especially as the disease advances.

Asymptomatic is an adjective categorising the medical conditions that patients carry but without experiencing their symptoms, despite an explicit diagnosis.
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.
Neuromyelitis optica spectrum disorders (NMOSD), including neuromyelitis optica (NMO), are autoimmune diseases characterized by acute inflammation of the optic nerve and the spinal cord (myelitis). Episodes of ON and myelitis can be simultaneous or successive. A relapsing disease course is common, especially in untreated patients. In more than 80% of cases, NMO is caused by immunoglobulin G autoantibodies to aquaporin 4 (anti-AQP4), the most abundant water channel protein in the central nervous system. A subset of anti-AQP4-negative cases is associated with antibodies against myelin oligodendrocyte glycoprotein (anti-MOG). Rarely, NMO may occur in the context of other autoimmune diseases or infectious diseases. In some cases, the etiology remains unknown.

The McDonald criteria are diagnostic criteria for multiple sclerosis (MS). These criteria are named after neurologist W. Ian McDonald who directed an international panel in association with the National Multiple Sclerosis Society (NMSS) of America and recommended revised diagnostic criteria for MS in April 2001. These new criteria intended to replace the Poser criteria and the older Schumacher criteria. They have undergone revisions in 2005, 2010 and 2017.

Multiple sclerosis is an inflammatory demyelinating disease of the CNS in which activated immune cells invade the central nervous system and cause inflammation, neurodegeneration, and tissue damage. The underlying cause is currently unknown. Current research in neuropathology, neuroimmunology, neurobiology, and neuroimaging, together with clinical neurology, provide support for the notion that MS is not a single disease but rather a spectrum.
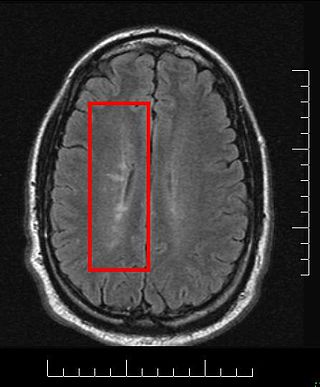
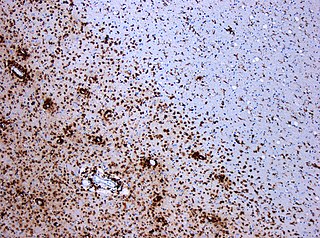
Multiple sclerosis and other demyelinating diseases of the central nervous system (CNS) produce lesions and glial scars or scleroses. They present different shapes and histological findings according to the underlying condition that produces them.
Inflammatory demyelinating diseases (IDDs), sometimes called Idiopathic (IIDDs) due to the unknown etiology of some of them, are a heterogenous group of demyelinating diseases - conditions that cause damage to myelin, the protective sheath of nerve fibers - that occur against the background of an acute or chronic inflammatory process. IDDs share characteristics with and are often grouped together under Multiple Sclerosis. They are sometimes considered different diseases from Multiple Sclerosis, but considered by others to form a spectrum differing only in terms of chronicity, severity, and clinical course.
Marburg acute multiple sclerosis, also known as Marburg multiple sclerosis or acute fulminant multiple sclerosis, is considered one of the multiple sclerosis borderline diseases, which is a collection of diseases classified by some as MS variants and by others as different diseases. Other diseases in this group are neuromyelitis optica (NMO), Balo concentric sclerosis, and Schilder's disease. The graver course is one form of malignant multiple sclerosis, with patients reaching a significant level of disability in less than five years from their first symptoms, often in a matter of months.

Multiple sclerosis can cause a variety of symptoms: changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty moving; difficulties with coordination and balance; problems in speech (dysarthria) or swallowing (dysphagia), visual problems, fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology. The main clinical measure in progression of the disability and severity of the symptoms is the Expanded Disability Status Scale or EDSS.
Research in multiple sclerosis may find new pathways to interact with the disease, improve function, curtail attacks, or limit the progression of the underlying disease. Many treatments already in clinical trials involve drugs that are used in other diseases or medications that have not been designed specifically for multiple sclerosis. There are also trials involving the combination of drugs that are already in use for multiple sclerosis. Finally, there are also many basic investigations that try to understand better the disease and in the future may help to find new treatments.
A clinically isolated syndrome (CIS) is a clinical situation of an individual's first neurological episode, caused by inflammation or demyelination of nerve tissue. An episode may be monofocal, in which symptoms present at a single site in the central nervous system, or multifocal, in which multiple sites exhibit symptoms. CIS with enough paraclinical evidence can be considered as a clinical stage of multiple sclerosis (MS). It can also be retrospectively diagnosed as a kind of MS when more evidence is available.

Tumefactive multiple sclerosis is a condition in which the central nervous system of a person has multiple demyelinating lesions with atypical characteristics for those of standard multiple sclerosis (MS). It is called tumefactive as the lesions are "tumor-like" and they mimic tumors clinically, radiologically and sometimes pathologically.
Diffuse myelinoclastic sclerosis, sometimes referred to as Schilder's disease, is a very infrequent neurodegenerative disease that presents clinically as pseudotumoural demyelinating lesions, making its diagnosis difficult. It usually begins in childhood, affecting children between 5 and 14 years old, but cases in adults are also possible.
Schumacher criteria are diagnostic criteria that were previously used for identifying multiple sclerosis (MS). Multiple sclerosis, understood as a central nervous system (CNS) condition, can be difficult to diagnose since its signs and symptoms may be similar to other medical problems. Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process especially in the first stages of the disease. Schumacher criteria were the first internationally recognized criteria for diagnosis, and introduced concepts still in use, as CDMS.

Current standards for diagnosing multiple sclerosis (MS) are based on the 2018 revision of McDonald criteria. They rely on MRI detection of demyelinating lesions in the CNS, which are distributed in space (DIS) and in time (DIT). It is also a requirement that any possible known disease that produces demyelinating lesions is ruled out before applying McDonald's criteria.

Multiple sclerosis (MS) can be pathologically defined as the presence of distributed glial scars (scleroses) in the central nervous system that must show dissemination in time (DIT) and in space (DIS) to be considered MS lesions.
Radiologically isolated syndrome (RIS) is a clinical situation in which a person has white matter lesions suggestive of multiple sclerosis (MS), as shown on an MRI scan that was done for reasons unrelated to MS symptoms. The nerve lesions in these people show dissemination in space with an otherwise normal neurological examination and without historical accounts of typical MS symptoms.
Several biomarkers for diagnosis of multiple sclerosis, disease evolution and response to medication are under research. While most of them are still under research, there are some of them already well stablished:
References
- ↑ Schumacher GA, Beebe G, Kibler RF, Kurland LT, Kurtzke JF, McDowell F, Nagler B, Sibley WA, Tourtellotte WW, Willmon TL (March 1965). "Problems of Experimental Trials of Therapy in Multiple Sclerosis: Report by the Panel on the Evaluation of Experimental Trials of Therapy in Multiple Sclerosis". Ann N Y Acad Sci. 122 (1): 552–568. Bibcode:1965NYASA.122..552S. doi:10.1111/j.1749-6632.1965.tb20235.x. PMID 14313512. S2CID 20718640.
- ↑ Christopher J. Lisanti, Patrick Asbach, and William G. Bradley, Jr. The Ependymal "Dot-Dash" Sign: An MR Imaging Finding of Early Multiple Sclerosis, AJNR Am J Neuroradiol 26:2033–2036, September 2005
- 1 2 Poser CM, Paty DW, Scheinberg L, et al. (March 1983). "New diagnostic criteria for multiple sclerosis: Guidelines for research protocols" (PDF). Annals of Neurology. 13 (3): 227–31. doi:10.1002/ana.410130302. PMID 6847134. S2CID 42781540. Archived from the original (PDF) on 2010-03-24. Retrieved 2009-11-05.
- 1 2 Izquierdo G, Hauw J-J, Lyon-Caen O; et al. (1985). "Value of multiple sclerosis diagnostic criteria: 70 Autopsy-confirmed cases". Arch Neurol. 42 (9): 848–850. doi:10.1001/archneur.1985.04060080026010. PMID 4026627.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Engell T (July 1988). "A clinico-pathoanatomical study of multiple sclerosis diagnosis". Acta Neurol. Scand. 78 (1): 39–44. doi: 10.1111/j.1600-0404.1988.tb03616.x . PMID 3176880. S2CID 22769204.
- ↑ Engell T (May 1989). "A clinical patho-anatomical study of clinically silent multiple sclerosis". Acta Neurol Scand. 79 (5): 428–30. doi: 10.1111/j.1600-0404.1989.tb03811.x . PMID 2741673. S2CID 21581253.
- ↑ Hakiki B, Goretti B, Portaccio E, Zipoli V, Amato MP (2008). "Subclinical MS: follow-up of four cases". European Journal of Neurology. 15 (8): 858–61. doi:10.1111/j.1468-1331.2008.02155.x. PMID 18507677. S2CID 27212599.
- ↑ Lebrun C, Bensa C, Debouverie M, et al. (2008). "Unexpected multiple sclerosis: follow-up of 30 patients with magnetic resonance imaging and clinical conversion profile". J Neurol Neurosurg Psychiatry. 79 (2): 195–198. doi:10.1136/jnnp.2006.108274. PMID 18202208. S2CID 11750372.
- ↑ Frisullo G, Nociti V, Iorio R, et al. (Dec 2008). "The persistency of high levels of pSTAT3 expression in circulating CD4+ T cells from CIS patients favors the early conversion to clinically defined multiple sclerosis". J. Neuroimmunol. 205 (1–2): 126–134. doi:10.1016/j.jneuroim.2008.09.003. PMID 18926576. S2CID 27303451.