Acute disseminated encephalomyelitis (ADEM), or acute demyelinating encephalomyelitis, is a rare autoimmune disease marked by a sudden, widespread attack of inflammation in the brain and spinal cord. As well as causing the brain and spinal cord to become inflamed, ADEM also attacks the nerves of the central nervous system and damages their myelin insulation, which, as a result, destroys the white matter. It is often triggered by a viral infection or specific non-routine vaccinations.

Transverse myelitis (TM) is a rare neurological condition in which the spinal cord is inflamed. Transverse implies that the inflammation extends horizontally across the spinal cord. Partial transverse myelitis and partial myelitis are terms sometimes used to specify inflammation that only affects part of the width of the spinal cord. TM is characterized by weakness and numbness of the limbs, deficits in sensation and motor skills, dysfunctional urethral and anal sphincter activities, and dysfunction of the autonomic nervous system that can lead to episodes of high blood pressure. Signs and symptoms vary according to the affected level of the spinal cord. The underlying cause of TM is unknown. The spinal cord inflammation seen in TM has been associated with various infections, immune system disorders, or damage to nerve fibers, by loss of myelin. As opposed to leukomyelitis which affects only the white matter, it affects the entire cross-section of the spinal cord. Decreased electrical conductivity in the nervous system can result.
Multiple sclerosis (MS), also known as encephalomyelitis disseminata, is a demyelinating disease in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This damage disrupts the ability of parts of the nervous system to transmit signals, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Specific symptoms can include double vision, blindness in one eye, muscle weakness and trouble with sensation or coordination. MS takes several forms, with new symptoms either occurring in isolated attacks or building up over time. Between attacks, symptoms may disappear completely; however, permanent neurological problems often remain, especially as the disease advances.
A demyelinating disease is any disease of the nervous system in which the myelin sheath of neurons is damaged. This damage impairs the conduction of signals in the affected nerves. In turn, the reduction in conduction ability causes deficiency in sensation, movement, cognition, or other functions depending on which nerves are involved.
Neuromyelitis optica spectrum disorders (NMOSD) is an etiologically heterogeneous syndrome predominantly characterized by acute inflammation of the optic nerve and the spinal cord (myelitis). Episodes of ON and myelitis can be simultaneous or successive. A relapsing disease course is common, especially in untreated patients. In more than 80% of cases, NMO is caused by immunoglobulin G autoantibodies to aquaporin 4 (anti-AQP4), the most abundant water channel protein in the central nervous system. A subset of anti-AQP4-negative cases is associated with antibodies to myelin oligodendrocyte glycoprotein (anti-MOG). Rarely, NMO may occur in the context of other autoimmune diseases or infectious diseases. In some cases, the etiology remains unknown.

The McDonald criteria are diagnostic criteria for multiple sclerosis (MS). These criteria are named after neurologist W. Ian McDonald who directed an international panel in association with the National Multiple Sclerosis Society (NMSS) of America and recommended revised diagnostic criteria for MS in April 2001. These new criteria intended to replace the Poser criteria and the older Schumacher criteria. They have undergone revisions in 2005, 2010 and 2017.

Multiple sclerosis is an inflammatory demyelinating disease of the CNS in which activated immune cells invade the central nervous system and cause inflammation, neurodegeneration, and tissue damage. The underlying cause is currently unknown. Current research in neuropathology, neuroimmunology, neurobiology, and neuroimaging, together with clinical neurology, provide support for the notion that MS is not a single disease but rather a spectrum.

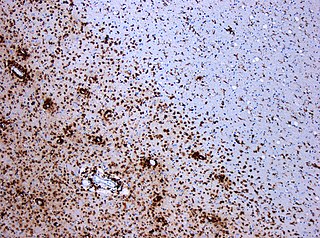
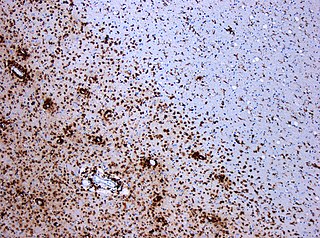
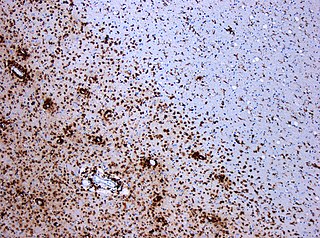
Multiple sclerosis and other demyelinating diseases of the central nervous system (CNS) produce lesions and glial scars or scleroses. They present different shapes and histological findings according to the underlying condition that produces them.
Inflammatory demyelinating diseases (IDDs), sometimes called Idiopathic (IIDDs) because the unknown etiology of some of them, and sometimes known as borderline forms of multiple sclerosis, is a collection of multiple sclerosis variants, sometimes considered different diseases, but considered by others to form a spectrum differing only in terms of chronicity, severity, and clinical course.

Multiple sclerosis can cause a variety of symptoms: changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty moving; difficulties with coordination and balance; problems in speech (dysarthria) or swallowing (dysphagia), visual problems, fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology. The main clinical measure in progression of the disability and severity of the symptoms is the Expanded Disability Status Scale or EDSS.
Research in multiple sclerosis may find new pathways to interact with the disease, improve function, curtail attacks, or limit the progression of the underlying disease. Many treatments already in clinical trials involve drugs that are used in other diseases or medications that have not been designed specifically for multiple sclerosis. There are also trials involving the combination of drugs that are already in use for multiple sclerosis. Finally, there are also many basic investigations that try to understand better the disease and in the future may help to find new treatments.
A clinically isolated syndrome (CIS) is a clinical situation of an individual's first neurological episode, caused by inflammation or demyelination of nerve tissue. An episode may be monofocal, in which symptoms present at a single site in the central nervous system, or multifocal, in which multiple sites exhibit symptoms. CIS with enough paraclinical evidence can be considered as a clinical stage of multiple sclerosis (MS). It can also be retrospectively diagnosed as a kind of MS when more evidence is available.

Tumefactive multiple sclerosis is a condition in which the central nervous system of a person has multiple demyelinating lesions with atypical characteristics for those of standard multiple sclerosis (MS). It is called tumefactive as the lesions are "tumor-like" and they mimic tumors clinically, radiologically and sometimes pathologically.
Diffuse myelinoclastic sclerosis, sometimes referred to as Schilder's disease, is a very infrequent neurodegenerative disease that presents clinically as pseudotumoural demyelinating lesions, making its diagnosis difficult. It usually begins in childhood, affecting children between 5 and 14 years old, but cases in adults are also possible.
Poser criteria are diagnostic criteria for multiple sclerosis (MS). They replaced the older Schumacher criteria, and now they are considered obsolete as McDonald criteria have superseded them. Nevertheless, some of the concepts introduced have remained in MS research, like CDMS, and newer criteria are often calibrated against them.

Current standard for diagnosing MS is based in the 2018 revision of McDonald criteria. They rely in MRI detection of demyelinating lesions in the CNS, which are distributed in space (DIS) and in time (DIT). It is also a requirement that any possible known disease that produces demyelinating lesions is ruled out before applying McDonald's criteria.

Multiple sclerosis (MS) can be pathologically defined as the presence of distributed glial scars (scleroses) in the central nervous system that must show dissemination in time (DIT) and in space (DIS) to be considered MS lesions.
MOG antibody disease, MOGAD or Anti-MOG associated encephalomyelitis is an inflammatory demyelinating disease of the central nervous system. Serum anti-myelin oligodendrocyte glycoprotein antibodies are present in up to half of patients with an acquired demyelinating syndrome and have been described in association with a range of phenotypic presentations, including acute disseminated encephalomyelitis, optic neuritis, transverse myelitis, and neuromyelitis optica.
Radiologically isolated syndrome (RIS) is a clinical situation in which a person has white matter lesions suggestive of multiple sclerosis (MS), as shown on an MRI scan that was done for reasons unrelated to MS symptoms. The nerve lesions in these people show dissemination in space with an otherwise normal neurological examination and without historical accounts of typical MS symptoms.
Several biomarkers for diagnosis of multiple sclerosis, disease evolution and response to medication are under research. While most of them are still under research, there are some of them already well stablished: