Acute disseminated encephalomyelitis (ADEM), or acute demyelinating encephalomyelitis, is a rare autoimmune disease marked by a sudden, widespread attack of inflammation in the brain and spinal cord. As well as causing the brain and spinal cord to become inflamed, ADEM also attacks the nerves of the central nervous system and damages their myelin insulation, which, as a result, destroys the white matter. The cause is often a trigger such as from viral infection or vaccinations.

Optic neuritis describes any condition that causes inflammation of the optic nerve; it may be associated with demyelinating diseases, or infectious or inflammatory processes.

Multiple sclerosis (MS) is an autoimmune disease resulting in damage to the insulating covers of nerve cells in the brain and spinal cord. As a demyelinating disease, MS disrupts the nervous system's ability to transmit signals, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Symptoms include double vision, vision loss, eye pain, muscle weakness, and loss of sensation or coordination. MS takes several forms, with new symptoms either occurring in isolated attacks or building up over time. In relapsing forms of MS symptoms may disappear completely between attacks, although some permanent neurological problems often remain, especially as the disease advances. In progressive forms of MS, bodily function slowly deteriorates once symptoms manifest and will steadily worsen if left untreated.
Neuromyelitis optica spectrum disorders (NMOSD) are a spectrum of autoimmune diseases characterized by acute inflammation of the optic nerve and the spinal cord (myelitis). Episodes of ON and myelitis can be simultaneous or successive. A relapsing disease course is common, especially in untreated patients.

Myelin oligodendrocyte glycoprotein (MOG) is a glycoprotein believed to be important in the myelination of nerves in the central nervous system (CNS). In humans this protein is encoded by the MOG gene. It is speculated to serve as a necessary "adhesion molecule" to provide structural integrity to the myelin sheath and is known to develop late on the oligodendrocyte.
Experimental autoimmune encephalomyelitis, sometimes experimental allergic encephalomyelitis (EAE), is an animal model of brain inflammation. It is an inflammatory demyelinating disease of the central nervous system (CNS). It is mostly used with rodents and is widely studied as an animal model of the human CNS demyelinating diseases, including multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM). EAE is also the prototype for T-cell-mediated autoimmune disease in general.
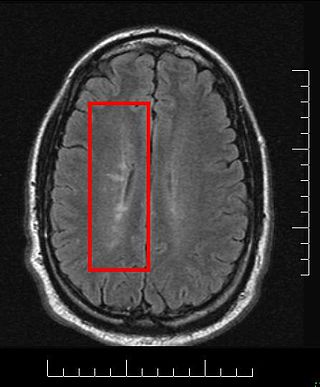
Multiple sclerosis and other demyelinating diseases of the central nervous system (CNS) produce lesions and glial scars or scleroses. They present different shapes and histological findings according to the underlying condition that produces them.
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease that affects the central nervous system (CNS). Several therapies for it exist, although there is no known cure.
Inflammatory demyelinating diseases (IDDs), sometimes called Idiopathic (IIDDs) due to the unknown etiology of some of them, are a heterogenous group of demyelinating diseases - conditions that cause damage to myelin, the protective sheath of nerve fibers - that occur against the background of an acute or chronic inflammatory process. IDDs share characteristics with and are often grouped together under Multiple Sclerosis. They are sometimes considered different diseases from Multiple Sclerosis, but considered by others to form a spectrum differing only in terms of chronicity, severity, and clinical course.

Baló's concentric sclerosis is a disease in which the white matter of the brain appears damaged in concentric layers, leaving the axis cylinder intact. It was described by József Mátyás Baló who initially named it "leuko-encephalitis periaxialis concentrica" from the previous definition, and it is currently considered one of the borderline forms of multiple sclerosis.
Research in multiple sclerosis may find new pathways to interact with the disease, improve function, curtail attacks, or limit the progression of the underlying disease. Many treatments already in clinical trials involve drugs that are used in other diseases or medications that have not been designed specifically for multiple sclerosis. There are also trials involving the combination of drugs that are already in use for multiple sclerosis. Finally, there are also many basic investigations that try to understand the disease better and in the future may help to find new treatments.

Tumefactive multiple sclerosis is a condition in which the central nervous system of a person has multiple demyelinating lesions with atypical characteristics for those of standard multiple sclerosis (MS). It is called tumefactive as the lesions are "tumor-like" and they mimic tumors clinically, radiologically and sometimes pathologically.
Diffuse myelinoclastic sclerosis, sometimes referred to as Schilder's disease, is a very infrequent neurodegenerative disease that presents clinically as pseudotumoural demyelinating lesions, making its diagnosis difficult. It usually begins in childhood, affecting children between 5 and 14 years old, but cases in adults are also possible.
Malignant multiple sclerosis is used to describe MS patients who reach significant level of disability in a short period of time. Malignant MS cases are not common, less than 5% of patients with MS experience this type of progression.

Current standards for diagnosing multiple sclerosis (MS) are based on the 2018 revision of McDonald criteria. They rely on MRI detection of demyelinating lesions in the CNS, which are distributed in space (DIS) and in time (DIT). It is also a requirement that any possible known disease that produces demyelinating lesions is ruled out before applying McDonald's criteria.
Chronic relapsing inflammatory optic neuropathy (CRION) is a form of recurrent optic neuritis that is steroid responsive and dependent. Patients typically present with pain associated with visual loss. CRION is a clinical diagnosis of exclusion, and other demyelinating, autoimmune, and systemic causes should be ruled out. An accurate antibody test which became available commercially in 2017 has allowed most patients previously diagnosed with CRION to be re-identified as having MOG antibody disease, which is not a diagnosis of exclusion. Early recognition is crucial given risks for severe visual loss and because it is treatable with immunosuppressive treatment such as steroids or B-cell depleting therapy. Relapse that occurs after reducing or stopping steroids is a characteristic feature.
MOG antibody disease (MOGAD) or MOG antibody-associated encephalomyelitis (MOG-EM) is an inflammatory demyelinating disease of the central nervous system. Serum anti-myelin oligodendrocyte glycoprotein antibodies are present in up to half of patients with an acquired demyelinating syndrome and have been described in association with a range of phenotypic presentations, including acute disseminated encephalomyelitis, optic neuritis, transverse myelitis, and neuromyelitis optica.
There are several ways for pharmaceuticals for treating multiple sclerosis (MS) to reach the market.
Anti-AQP4 diseases, are a group of diseases characterized by auto-antibodies against aquaporin 4.
Brenda Banwell is Chief of the Division of Neurology and Co-Director of the Neuroscience Center, and Professor of Neurology at Children's Hospital of Philadelphia and holder of the Grace R. Loeb Endowed Chair in Neurosciences. She also holds the title of Professor of Pediatrics and Neurology at the Perelman School of Medicine at the University of Pennsylvania.