Related Research Articles
Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of the use of emergency medication on site. It typically causes more than one of the following: an itchy rash, throat closing due to swelling that can obstruct or stop breathing; severe tongue swelling that can also interfere with or stop breathing; shortness of breath, vomiting, lightheadedness, loss of consciousness, low blood pressure, and medical shock. These symptoms typically start in minutes to hours and then increase very rapidly to life-threatening levels. Urgent medical treatment is required to prevent serious harm and death, even if the patient has used an epipen or has taken other medications in response, and even if symptoms appear to be improving.

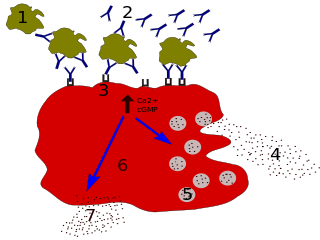
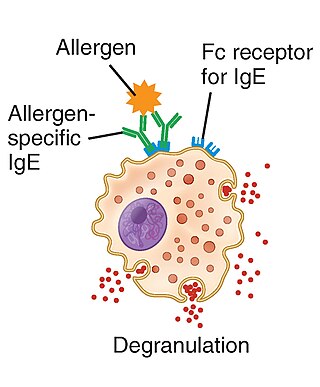
A mast cell is a resident cell of connective tissue that contains many granules rich in histamine and heparin. Specifically, it is a type of granulocyte derived from the myeloid stem cell that is a part of the immune and neuroimmune systems. Mast cells were discovered by Paul Ehrlich in 1877. Although best known for their role in allergy and anaphylaxis, mast cells play an important protective role as well, being intimately involved in wound healing, angiogenesis, immune tolerance, defense against pathogens, and vascular permeability in brain tumors.
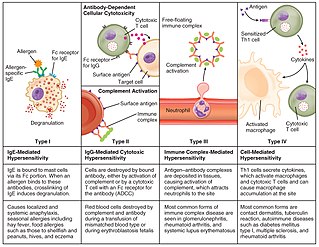
Hypersensitivity is an abnormal physiological condition in which there is an undesirable and adverse immune response to an antigen. It is an abnormality in the immune system that causes immune diseases including allergies and autoimmunity. It is caused by many types of particles and substances from the external environment or from within the body that are recognized by the immune cells as antigens. The immune reactions are usually referred to as an over-reaction of the immune system and they are often damaging and uncomfortable.

Basophils are a type of white blood cell. Basophils are the least common type of granulocyte, representing about 0.5% to 1% of circulating white blood cells. They are the largest type of granulocyte. They are responsible for inflammatory reactions during immune response, as well as in the formation of acute and chronic allergic diseases, including anaphylaxis, asthma, atopic dermatitis and hay fever. They also produce compounds that coordinate immune responses, including histamine and serotonin that induce inflammation, and heparin that prevents blood clotting, although there are less than that found in mast cell granules. Mast cells were once thought to be basophils that migrated from the blood into their resident tissues, but they are now known to be different types of cells.
Immunoglobulin E (IgE) is a type of antibody that has been found only in mammals. IgE is synthesised by plasma cells. Monomers of IgE consist of two heavy chains and two light chains, with the ε chain containing four Ig-like constant domains (Cε1–Cε4). IgE is thought to be an important part of the immune response against infection by certain parasitic worms, including Schistosoma mansoni, Trichinella spiralis, and Fasciola hepatica. IgE is also utilized during immune defense against certain protozoan parasites such as Plasmodium falciparum. IgE may have evolved as a defense to protect against venoms.

Rhinitis, also known as coryza, is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.
Type I hypersensitivity, in the Gell and Coombs classification of allergic reactions, is an allergic reaction provoked by re-exposure to a specific type of antigen referred to as an allergen. Type I is distinct from type II, type III and type IV hypersensitivities. The relevance of the Gell and Coombs classification of allergic reactions has been questioned in the modern-day understanding of allergy, and it has limited utility in clinical practice.

Omalizumab, sold under the brand name Xolair among others, is an injectable medication to treat severe persistent allergic forms of asthma, nasal polyps, urticaria (hives), and immunoglobulin E-mediated food allergy.

Ketotifen is an antihistamine medication and a mast cell stabilizer used to treat allergic conditions such as conjunctivitis, asthma, and urticaria (hives). Ketotifen is available in ophthalmic and oral forms: the ophthalmic form relieves eye itchiness and irritation associated with seasonal allergies, while the oral form helps prevent systemic conditions such as asthma attacks and allergic reactions. In addition to treating allergies, ketotifen has shown efficacy in managing systemic mast cell diseases such as mastocytosis and mast cell activation syndrome (MCAS), which involve abnormal accumulation or activation of mast cells throughout the body. Ketotifen is also used for other allergic-type conditions like atopic dermatitis (eczema) and food allergies.
In immunology, the Arthus reaction is a type of local type III hypersensitivity reaction. Type III hypersensitivity reactions are immune complex-mediated, and involve the deposition of antigen/antibody complexes mainly in the vascular walls, serosa, and glomeruli. This reaction is usually encountered in experimental settings following the injection of antigens.

The high-affinity IgE receptor, also known as FcεRI, or Fc epsilon RI, is the high-affinity receptor for the Fc region of immunoglobulin E (IgE), an antibody isotype involved in allergy disorders and parasite immunity. FcεRI is a tetrameric receptor complex that binds Fc portion of the ε heavy chain of IgE. It consists of one alpha, one beta, and two gamma chains connected by two disulfide bridges on mast cells and basophils. It lacks the beta subunit on other cells. It is constitutively expressed on mast cells and basophils and is inducible in eosinophils.

Mas-related G-protein coupled receptor member X2 is a protein that in humans is encoded by the MRGPRX2 gene. It is most abundant on cutaneous mast cells, sensory neurons, and keratinocytes.

Allergic symptoms are caused by an initial systemic histamine release by activated basophils and mast cells, that may lead to shock with laryngeal edema, lower-airway obstruction and hypotension. This is why basophils are considered with mast cells to be the key cells in allergic diseases.
One of the most prevalent forms of adverse drug reactions is cutaneous reactions, with drug-induced urticaria ranking as the second most common type, preceded by drug-induced exanthems. Urticaria, commonly known as hives, manifests as weals, itching, burning, redness, swelling, and angioedema—a rapid swelling of lower skin layers, often more painful than pruritic. These symptoms may occur concurrently, successively, or independently. Typically, when a drug triggers urticaria, symptoms manifest within 24 hours of ingestion, aiding in the identification of the causative agent. Urticaria symptoms usually subside within 1–24 hours, while angioedema may take up to 72 hours to resolve completely.
Kounis syndrome is defined as acute coronary syndrome caused by an allergic reaction or a strong immune reaction to a drug or other substance. It is a rare syndrome with authentic cases reported in 130 males and 45 females, as reviewed in 2017; however, the disorder is suspected of being commonly overlooked and therefore much more prevalent. Mast cell activation and release of inflammatory cytokines as well as other inflammatory agents from the reaction leads to spasm of the arteries leading to the heart muscle or a plaque breaking free and blocking one or more of those arteries.
Mast cell activation syndrome (MCAS) is a term referring to one of two types of mast cell activation disorder (MCAD); the other type is idiopathic MCAD. MCAS is an immunological condition in which mast cells inappropriately and excessively release chemical mediators, resulting in a range of chronic symptoms, sometimes including anaphylaxis or near-anaphylaxis attacks. Primary symptoms include cardiovascular, dermatological, gastrointestinal, neurological and respiratory problems.
NSAIDhypersensitivity reactions encompass a broad range of allergic or allergic-like symptoms that occur within minutes to hours after ingesting aspirin or other NSAID nonsteroidal anti-inflammatory drugs. Hypersensitivity drug reactions differ from drug toxicity reactions in that drug toxicity reactions result from the pharmacological action of a drug, are dose-related, and can occur in any treated individual. Hypersensitivity reactions are idiosyncratic reactions to a drug. Although the term NSAID was introduced to signal a comparatively low risk of adverse effects, NSAIDs do evoke a broad range of hypersensitivity syndromes. These syndromes have recently been classified by the European Academy of Allergy and Clinical Immunology Task Force on NSAIDs Hypersensitivity.

Proxicromil is a detergent-like, lipophilic oral medication developed in the late 1970s that was not admitted on the market because of its possible carcinogenic effects. It suppresses allergic reactions by binding to FcεRI receptor in mast cells, thereby inhibiting production of histamines. It is absorbed through the gastrointestinal tract, and has been proven hepatotoxic for dogs as a result of its accumulation in biliary canaliculi.
Lirentelimab is a humanized nonfucosylated monoclonal antibody that targets sialic acid-binding Ig-like lectin 8 (SIGLEC8). In a randomized clinical trial, lirentelimab was found to improve eosinophil counts and symptoms in individuals with eosinophilic gastritis and duodenitis. Adverse reactions include infusion reactions, which are mild to moderate and typically occur following the first infusion.
Anti-allergic agents are medications used to treat allergic reactions. Anti-allergic agents have existed since 3000 B.C in countries such as China and Egypt. It was not until 1933 when antihistamines, the first type of anti-allergic agents, were developed. Common allergic diseases include allergic rhinitis, allergic asthma and atopic dermatitis with varying symptoms, including runny nose, watery eyes, itchiness, coughing, and shortness of breath. More than one-third of the world's population is currently being affected by one or more allergic conditions.
References
- ↑ Zuberbier, Torsten (2001). "The Role of Allergens and Pseudoallergens in Urticaria". Journal of Investigative Dermatology Symposium Proceedings. 6 (2). Elsevier BV: 132–134. doi: 10.1046/j.0022-202x.2001.00024.x . ISSN 1087-0024. PMID 11764298.
- 1 2 3 Rich, Robert R.; Fleisher, Thomas A.; Schroeder, Harry W.; Weyand, Cornelia M.; Corry, David B.; Puck, Jennifer, eds. (2023). Clinical immunology: principles and practice (6th ed.). Amsterdam, The Netherlands: Elsevier. ISBN 978-0-7020-8165-1. OCLC 1295106160.
- ↑ Grattan, Clive E.H.; Borzova, Elena (2019). "Urticaria, Angioedema, and Anaphylaxis". Clinical Immunology. Elsevier. pp. 585–600.e1. doi:10.1016/b978-0-7020-6896-6.00042-9. ISBN 978-0-7020-6896-6.
- ↑ Reese, Imke; Zuberbier, Torsten; Bunselmeyer, Britta; Erdmann, Stephan; Henzgen, Margot; Fuchs, Thomas; Jäger, Lothar; Kleine‐Tebbe, Jörg; Lepp, Ute; Niggemann, Bodo; Raithel, Martin; Saloga, Joachim; Vieths, Stephan; Werfel, Thomas (2009). "Diagnostic approach for suspected pseudoallergic reaction to food ingredients". JDDG: Journal der Deutschen Dermatologischen Gesellschaft. 7 (1): 70–77. doi:10.1111/j.1610-0387.2008.06894.x. ISSN 1610-0379. PMID 19054425. S2CID 23773448.
- ↑ Cleveland Clinic medical professional (2017-09-12). "Food Challenge Tests". Cleveland Clinic. Retrieved 2024-06-21.
- ↑ He, Shao-heng; Zhang, Hui-yun; Zeng, Xiao-ning; Chen, Dong; Yang, Ping-chang (August 26, 2013). "Mast cells and basophils are essential for allergies: mechanisms of allergic inflammation and a proposed procedure for diagnosis". Acta Pharmacologica Sinica. 34 (10). Springer Science and Business Media LLC: 1270–1283. doi:10.1038/aps.2013.88. ISSN 1671-4083. PMC 4002163 . PMID 23974516.
- ↑ Toncić, Ruzica Jurakić; Marinović, Branka; Lipozencić, Jasna (2009). "Nonallergic hypersensitivity to nonsteroidal antiinflammatory drugs, angiotensin-converting enzyme inhibitors, radiocontrast media, local anesthetics, volume substitutes and medications used in general anesthesia". Acta Dermatovenerologica Croatica. 17 (1): 54–69. PMID 19386216.
- ↑ Wang, Zhiguo; Wang, Danqiao; Sui, Yu; Cui, Haifeng; Yu, Youhua (2012). "Experimental study on anaphylaxis of Qingkailing injection and its components on Beagle dogs". Journal of Traditional Chinese Medicine. 32 (4). Elsevier BV: 641–645. doi: 10.1016/s0254-6272(13)60085-0 . ISSN 0254-6272. PMID 23427403.
- ↑ Baker, Mark D.; Gullett, John P. (2015). "Ultrasound-Guided Femoral Nerve Blocks". Pediatric Emergency Care. 31 (12). Ovid Technologies (Wolters Kluwer Health): 864–868. doi:10.1097/pec.0000000000000634. ISSN 0749-5161. PMID 26626896. S2CID 5150857.
- ↑ Becker, Daniel E. (December 1, 2013). "Drug Allergies and Implications for Dental Practice". Anesthesia Progress. 60 (4). American Dental Society of Anesthesiology (ADSA): 188–197. doi:10.2344/0003-3006-60.4.188. ISSN 0003-3006. PMC 3891459 . PMID 24423421.
- ↑ Wang, Hong (2011). "Agents that induce pseudo-allergic reaction". Drug Discoveries & Therapeutics. 5 (5). International Research and Cooperation Association for Bio & Socio-Sciences Advancement (IRCA-BSSA): 211–219. doi: 10.5582/ddt.2011.v5.5.211 . ISSN 1881-7831. PMID 22466368.
- ↑ "1868-2020: Supporting general practitioners for more than 150 years". The Practitioner. September 24, 2015. Retrieved December 20, 2023.
- ↑ Yoo, Hye-Soo; Yang, Eun-Mi; Kim, Mi-Ae; Hwang, Sun-Hyuk; Shin, Yoo-Seob; Ye, Young-Min; Nahm, Dong-Ho; Park, Hae-Sim (2014). "A Case of Codeine Induced Anaphylaxis via Oral Route". Allergy, Asthma & Immunology Research. 6 (1). The Korean Academy of Asthma, Allergy and Clinical Immunology and The Korean Academy of Pediatric Al: 95. doi:10.4168/aair.2014.6.1.95. ISSN 2092-7355. PMC 3881408 .
- ↑ Sheen, C. H.; Schleimer, R. P.; Kulka, M. (April 12, 2007). "Codeine induces human mast cell chemokine and cytokine production: involvement of G‐protein activation". Allergy. 62 (5). Wiley: 532–538. doi:10.1111/j.1398-9995.2007.01345.x. ISSN 0105-4538. PMC 2199376 . PMID 17441793.
- ↑ McNeil, Benjamin D.; Pundir, Priyanka; Meeker, Sonya; Han, Liang; Undem, Bradley J.; Kulka, Marianna; Dong, Xinzhong (March 2015). "Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions". Nature. 519 (7542): 237–241. doi:10.1038/nature14022. ISSN 0028-0836. PMC 4359082 . PMID 25517090.
- ↑ Ring, J; Messmer, K (1977). "Incidence and Severity of Anaphylactoid Reactions to Colloid Volume Substitutes". The Lancet. 309 (8009). Elsevier BV: 466–469. doi:10.1016/s0140-6736(77)91953-5. ISSN 0140-6736. S2CID 37201704.
- ↑ Zhang, Bo; Li, Qin; Shi, Chenyang; Zhang, Xinyue (November 15, 2017). "Drug-Induced Pseudoallergy: A Review of the Causes and Mechanisms". Pharmacology. 101 (1–2). S. Karger AG: 104–110. doi: 10.1159/000479878 . ISSN 0031-7012. PMID 29136631.
- ↑ Szebeni, Janos; Alving, Carl R.; Savay, Sandor; Barenholz, Yechezkel; Priev, Aba; Danino, Dganit; Talmon, Yeshayahu (2001). "Formation of complement-activating particles in aqueous solutions of Taxol: possible role in hypersensitivity reactions". International Immunopharmacology. 1 (4). Elsevier BV: 721–735. doi:10.1016/s1567-5769(01)00006-6. ISSN 1567-5769. PMID 11357884.