Related Research Articles
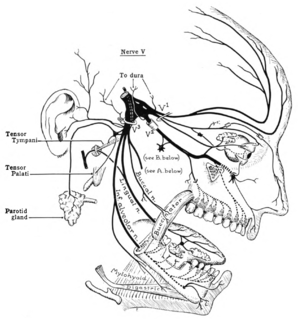
The trigeminal nerve (the fifth cranial nerve, or simply CN V) is a nerve responsible for sensation in the face and motor functions such as biting and chewing; it is the most complex of the cranial nerves. Its name ("trigeminal" = tri-, or three, and - geminus, or twin: thrice-twinned) derives from each of the two nerves (one on each side of the pons) having three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). The ophthalmic and maxillary nerves are purely sensory, whereas the mandibular nerve supplies motor as well as sensory (or "cutaneous") functions. Adding to the complexity of this nerve is that autonomic nerve fibers as well as special sensory fibers (taste) are contained within it.
Alien hand syndrome (AHS) or Dr. Strangelove syndrome is a category of conditions in which a person experiences their limbs acting seemingly on their own, without conscious control over the actions. There are a variety of clinical conditions that fall under this category, which most commonly affects the left hand. There are many similar terms for the various forms of the condition, but they are often used inappropriately. The afflicted person may sometimes reach for objects and manipulate them without wanting to do so, even to the point of having to use the controllable hand to restrain the alien hand. While under normal circumstances, thought, as intent, and action can be assumed to be deeply mutually entangled, the occurrence of alien hand syndrome can be usefully conceptualized as a phenomenon reflecting a functional "disentanglement" between thought and action.

The sensory nervous system is a part of the nervous system responsible for processing sensory information. A sensory system consists of sensory neurons, neural pathways, and parts of the brain involved in sensory perception. Commonly recognized sensory systems are those for vision, hearing, touch, taste, smell, and balance. In short, senses are transducers from the physical world to the realm of the mind where we interpret the information, creating our perception of the world around us.

The parietal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The parietal lobe is positioned above the temporal lobe and behind the frontal lobe and central sulcus.

The spinothalamic tract is a sensory pathway to the thalamus. From the ventral posterolateral nucleus in the thalamus, sensory information is relayed upward to the somatosensory cortex of the postcentral gyrus.

The primary somatosensory cortex is located in the postcentral gyrus, and is part of the somatosensory system. It was initially defined from surface stimulation studies of Wilder Penfield, and parallel surface potential studies of Bard, Woolsey, and Marshall. Although initially defined to be roughly the same as Brodmann areas 3, 1 and 2, more recent work by Kaas has suggested that for homogeny with other sensory fields only area 3 should be referred to as "primary somatosensory cortex", as it receives the bulk of the thalamocortical projections from the sensory input fields.
Stereognosis is the ability to perceive and recognize the form of an object in the absence of visual and auditory information, by using tactile information to provide cues from texture, size, spatial properties, and temperature, etc. In humans, this sense, along with tactile spatial acuity, vibration perception, texture discrimination and proprioception, is mediated by the dorsal column-medial lemniscus pathway of the central nervous system. Stereognosis tests determine whether or not the parietal lobe of the brain is intact. Typically, these tests involved having the patient identify common objects placed in their hand without any visual cues. Stereognosis is a higher cerebral associative cortical function.
Phantom pain is a perception that an individual experiences relating to a limb or an organ that is not physically part of the body. Limb loss is a result of either removal by amputation or congenital limb deficiency. However, phantom limb sensations can also occur following nerve avulsion or spinal cord injury.

An aura is a perceptual disturbance experienced by some with epilepsy or migraine. An epileptic aura is a seizure.
Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.
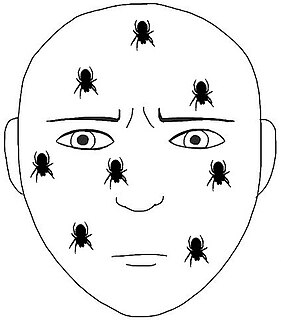
Cutaneous innervation refers to the area of the skin which is supplied by a specific cutaneous nerve.
Focal neurologic signs also known as focal neurological deficits or focal CNS signs are impairments of nerve, spinal cord, or brain function that affects a specific region of the body, e.g. weakness in the left arm, the right leg, paresis, or plegia.
Pallesthesia, or vibratory sensation, is the ability to perceive vibration. This sensation, often conducted through skin and bone, is usually generated by mechanoreceptors such as Pacinian corpuscles, Merkel disk receptors, and tactile corpuscles. All of these receptors stimulate an action potential in afferent nerves found in various layers of the skin and body. The afferent neuron travels to the spinal column and then to the brain where the information is processed. Damage to the peripheral nervous system or central nervous system can result in a decline or loss of pallesthesia.
Tactile discrimination is the ability to differentiate information through the sense of touch. The somatosensory system is the nervous system pathway that is responsible for this essential survival ability used in adaptation. There are various types of tactile discrimination. One of the most well known and most researched is two-point discrimination, the ability to differentiate between two different tactile stimuli which are relatively close together. Other types of discrimination like graphesthesia and spatial discrimination also exist but are not as extensively researched. Tactile discrimination is something that can be stronger or weaker in different people and two major conditions, chronic pain and blindness, can affect it greatly. Blindness increases tactile discrimination abilities which is extremely helpful for tasks like reading braille. In contrast, chronic pain conditions, like arthritis, decrease a person's tactile discrimination. One other major application of tactile discrimination is in new prosthetics and robotics which attempt to mimic the abilities of the human hand. In this case tactile sensors function similarly to mechanoreceptors in a human hand to differentiate tactile stimuli.

The somatosensory system is a part of the sensory nervous system. The somatosensory system is a complex system of sensory neurons and neural pathways that responds to changes at the surface or inside the body. The axons of sensory neurons connect with, or respond to, various receptor cells. These sensory receptor cells are activated by different stimuli such as heat and nociception, giving a functional name to the responding sensory neuron, such as a thermoreceptor which carries information about temperature changes. Other types include mechanoreceptors, chemoreceptors, and nociceptors which send signals along a sensory nerve to the spinal cord where they may be processed by other sensory neurons and then relayed to the brain for further processing. Sensory receptors are found all over the body including the skin, epithelial tissues, muscles, bones and joints, internal organs, and the cardiovascular system.
Extinction is a neurological disorder that impairs the ability to perceive multiple stimuli of the same type simultaneously. Extinction is usually caused by damage resulting in lesions on one side of the brain. Those who are affected by extinction have a lack of awareness in the contralesional side of space and a loss of exploratory search and other actions normally directed toward that side.
Amorphosynthesis, also called a hemi-sensory deficit, is a neuropsychological condition in which a patient experiences unilateral inattention to sensory input. This phenomenon is frequently associated with damage to the right cerebral hemisphere resulting in severe sensory deficits that are observed on the contralesional (left) side of the body. A right-sided deficit is less commonly observed and the effects are reported to be temporary and minor. Evidence suggests that the right cerebral hemisphere has a dominant role in attention and awareness to somatic sensations through ipsilateral and contralateral stimulation. In contrast, the left cerebral hemisphere is activated only by contralateral stimuli. Thus, the left and right cerebral hemispheres exhibit redundant processing to the right-side of the body and a lesion to the left cerebral hemisphere can be compensated by the ipsiversive processes of the right cerebral hemisphere. For this reason, right-sided amorphosynthesis is less often observed and is generally associated with bilateral lesions.
Somatosensory evoked potential is the electrical activity of the brain that results from the stimulation of touch. SEP tests measure that activity and are a useful, noninvasive means of assessing somatosensory system functioning. By combining SEP recordings at different levels of the somatosensory pathways, it is possible to assess the transmission of the afferent volley from the periphery up to the cortex. SEP components include a series of positive and negative deflections that can be elicited by virtually any sensory stimuli. For example, SEPs can be obtained in response to a brief mechanical impact on the fingertip or to air puffs. However, SEPs are most commonly elicited by bipolar transcutaneous electrical stimulation applied on the skin over the trajectory of peripheral nerves of the upper limb or lower limb, and then recorded from the scalp. In general, somatosensory stimuli evoke early cortical components, generated in the contralateral primary somatosensory cortex (S1), related to the processing of the physical stimulus attributes. About 100 ms after stimulus application, additional cortical regions are activated, such as the secondary somatosensory cortex (S2), and the posterior parietal and frontal cortices, marked by a parietal P100 and bilateral frontal N140. SEPs are routinely used in neurology today to confirm and localize sensory abnormalities, to identify silent lesions and to monitor changes during surgical procedures.
Cortical remapping, also referred to as cortical reorganization, is the process by which an existing cortical map is affected by a stimulus resulting in the creating of a 'new' cortical map. Every part of the body is connected to a corresponding area in the brain which creates a cortical map. When something happens to disrupt the cortical maps such as an amputation or a change in neuronal characteristics, the map is no longer relevant. The part of the brain that is in charge of the amputated limb or neuronal change will be dominated by adjacent cortical regions that are still receiving input, thus creating a remapped area. Remapping can occur in the sensory or motor system. The mechanism for each system may be quite different. Cortical remapping in the somatosensory system happens when there has been a decrease in sensory input to the brain due to deafferentation or amputation, as well as a sensory input increase to an area of the brain. Motor system remapping receives more limited feedback that can be difficult to interpret.
Tactile hallucination is the false perception of tactile sensory input that creates a hallucinatory sensation of physical contact with an imaginary object. It is caused by the faulty integration of the tactile sensory neural signals generated in the spinal cord and the thalamus and sent to the primary somatosensory cortex (SI) and secondary somatosensory cortex (SII). Tactile hallucinations are recurrent symptoms of neurological diseases such as schizophrenia, Parkinson's disease, Ekbom's syndrome and delerium tremens. Patients who experience phantom limb pains also experience a type of tactile hallucination. Tactile hallucinations are also caused by drugs such as cocaine and alcohol.
References
- 1 2 H., Ropper, Allan (2014-05-16). Adams and Victor's principles of neurology. Samuels, Martin A.,, Klein, Joshua (Tenth ed.). New York. ISBN 9780071794794. OCLC 857402060.
- 1 2 Augustine, James R. (2008). Human Neuroanatomy. San Diego, CA: Academic Press. p. 360. ISBN 978-0-12-068251-5.