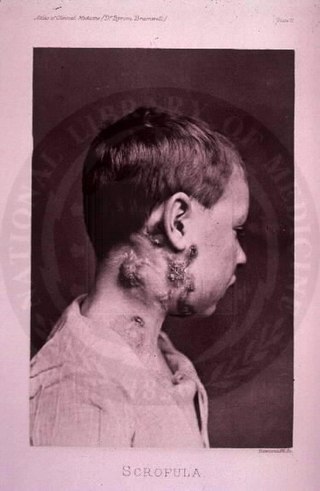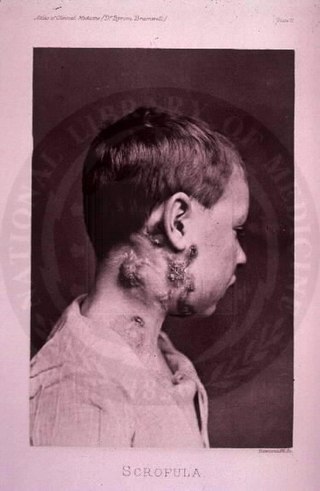
The disease mycobacterial cervical lymphadenitis, also known as scrofula and historically as king's evil, involves a lymphadenitis of the cervical lymph nodes associated with tuberculosis as well as nontuberculous (atypical) mycobacteria.

Castlemandisease (CD) describes a group of rare lymphoproliferative disorders that involve enlarged lymph nodes, and a broad range of inflammatory symptoms and laboratory abnormalities. Whether Castleman disease should be considered an autoimmune disease, cancer, or infectious disease is currently unknown.

Tumors of the hematopoietic and lymphoid tissues or tumours of the haematopoietic and lymphoid tissues are tumors that affect the blood, bone marrow, lymph, and lymphatic system. Because these tissues are all intimately connected through both the circulatory system and the immune system, a disease affecting one will often affect the others as well, making aplasia, myeloproliferation and lymphoproliferation closely related and often overlapping problems. While uncommon in solid tumors, chromosomal translocations are a common cause of these diseases. This commonly leads to a different approach in diagnosis and treatment of hematological malignancies. Hematological malignancies are malignant neoplasms ("cancer"), and they are generally treated by specialists in hematology and/or oncology. In some centers "hematology/oncology" is a single subspecialty of internal medicine while in others they are considered separate divisions. Not all hematological disorders are malignant ("cancerous"); these other blood conditions may also be managed by a hematologist.

Lymphadenopathy or adenopathy is a disease of the lymph nodes, in which they are abnormal in size or consistency. Lymphadenopathy of an inflammatory type is lymphadenitis, producing swollen or enlarged lymph nodes. In clinical practice, the distinction between lymphadenopathy and lymphadenitis is rarely made and the words are usually treated as synonymous. Inflammation of the lymphatic vessels is known as lymphangitis. Infectious lymphadenitis affecting lymph nodes in the neck is often called scrofula.

POEMS syndrome is a rare paraneoplastic syndrome caused by a clone of aberrant plasma cells. The name POEMS is an acronym for some of the disease's major signs and symptoms, as is PEP.

Invasive carcinoma of no special type (NST) is also referred to as invasive ductal carcinoma or infiltrating ductal carcinoma(IDC) and invasive ductal carcinoma, not otherwise specified (NOS). Each of these terms represents to the same disease entity, but for international audiences this article will use invasive carcinoma NST because it is the preferred term of the World Health Organization (WHO).

Lymphangiomas are malformations of the lymphatic system characterized by lesions that are thin-walled cysts; these cysts can be macroscopic, as in a cystic hygroma, or microscopic. The lymphatic system is the network of vessels responsible for returning to the venous system excess fluid from tissues as well as the lymph nodes that filter this fluid for signs of pathogens. These malformations can occur at any age and may involve any part of the body, but 90% occur in children less than 2 years of age and involve the head and neck. These malformations are either congenital or acquired. Congenital lymphangiomas are often associated with chromosomal abnormalities such as Turner syndrome, although they can also exist in isolation. Lymphangiomas are commonly diagnosed before birth using fetal ultrasonography. Acquired lymphangiomas may result from trauma, inflammation, or lymphatic obstruction.

Anaplastic thyroid cancer (ATC), also known as anaplastic thyroid carcinoma, is an aggressive form of thyroid cancer characterized by uncontrolled growth of cells in the thyroid gland. This form of cancer generally carries a very poor prognosis due to its aggressive behavior and resistance to cancer treatments. The cells of anaplastic thyroid cancer are highly abnormal and usually no longer resemble the original thyroid cells and have poor differentiation.
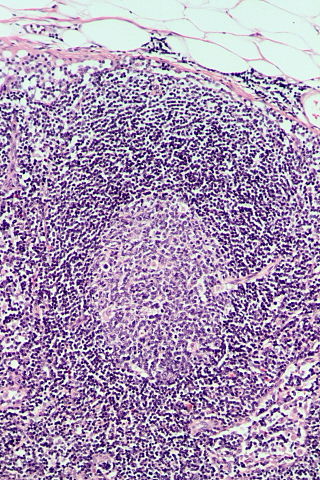
Lymphoid hyperplasia is the rapid proliferation of normal lymphocytic cells that resemble lymph tissue which may occur with bacterial or viral infections. The growth is termed hyperplasia which may result in enlargement of various tissue including an organ, or cause a cutaneous lesion.

Kimura's disease is a benign rare chronic inflammatory disorder. Its primary symptoms are subdermal lesions in the head or neck or painless unilateral inflammation of cervical lymph nodes.
Siltuximab is a chimeric monoclonal antibody. It binds to interleukin-6. Siltuximab has been investigated for the treatment of neoplastic diseases: metastatic renal cell cancer, prostate cancer, other types of cancer, and for Castleman's disease.

Marginal zone B-cell lymphomas, also known as marginal zone lymphomas (MZLs), are a heterogeneous group of lymphomas that derive from the malignant transformation of marginal zone B-cells. Marginal zone B cells are innate lymphoid cells that normally function by rapidly mounting IgM antibody immune responses to antigens such as those presented by infectious agents and damaged tissues. They are lymphocytes of the B-cell line that originate and mature in secondary lymphoid follicles and then move to the marginal zones of mucosa-associated lymphoid tissue, the spleen, or lymph nodes. Mucosa-associated lymphoid tissue is a diffuse system of small concentrations of lymphoid tissue found in various submucosal membrane sites of the body such as the gastrointestinal tract, mouth, nasal cavity, pharynx, thyroid gland, breast, lung, salivary glands, eye, skin and the human spleen.

Cervical lymphadenopathy refers to lymphadenopathy of the cervical lymph nodes. The term lymphadenopathy strictly speaking refers to disease of the lymph nodes, though it is often used to describe the enlargement of the lymph nodes. Similarly, the term lymphadenitis refers to inflammation of a lymph node, but often it is used as a synonym of lymphadenopathy.
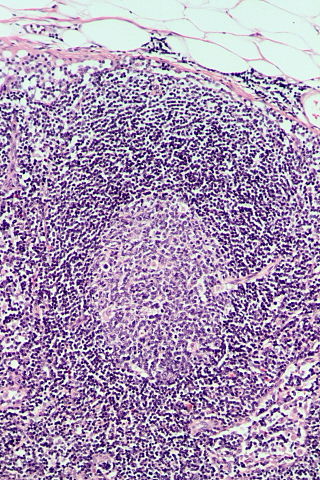
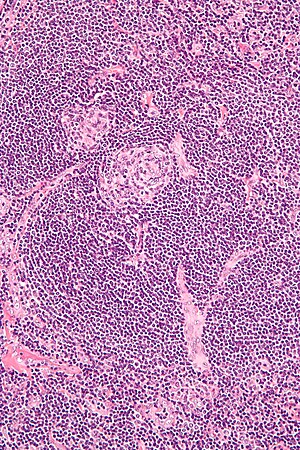
Follicular hyperplasia (FH) is a type of lymphoid hyperplasia and is classified as a lymphadenopathy, which means a disease of the lymph nodes. It is caused by a stimulation of the B cell compartment and by abnormal cell growth of secondary follicles. This typically occurs in the cortex without disrupting the lymph node capsule. The follicles are pathologically polymorphous, are often contrasting and varying in size and shape. Follicular hyperplasia is distinguished from follicular lymphoma in its polyclonality and lack of bcl-2 protein expression, whereas follicular lymphoma is monoclonal, and expresses bcl-2.
Large B-cell lymphoma arising in HHV8-associated multicentric Castleman's disease is a type of large B-cell lymphoma, recognized in the WHO 2008 classification. It is sometimes called the plasmablastic form of multicentric Castleman disease. It has sometimes been confused with plasmablastic lymphoma in the literature, although that is a dissimilar specific entity. It has variable CD20 expression and unmutated immunoglobulin variable region genes.
Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH) is a diffuse parenchymal lung disease which often presents with symptoms of cough and shortness of breath. The pathological definition published by the World Health Organization is “a generalized proliferation of scattered single cells, small nodules, or linear proliferations of pulmonary neuroendocrine (PNE) cells that may be confined to the bronchial and bronchiolar epithelium.” The true prevalence of this disease is not known. To date, just under 200 cases have been reported in the literature. However, with an increase in recognition of this disease by radiologists and pulmonologists, the number of cases has been increasing. DIPNECH predominantly affects middle-aged women with slowly progressive lung obstruction. DIPNECH is usually discovered in one of two ways: 1) as an unexpected finding following a lung surgery; or 2) by evaluation of a patient in a pulmonary clinic with longstanding, unexplained symptoms.

Human herpesvirus 8 associated multicentric Castleman disease is a subtype of Castleman disease, a group of rare lymphoproliferative disorders characterized by lymph node enlargement, characteristic features on microscopic analysis of enlarged lymph node tissue, and a range of symptoms and clinical findings.

Idiopathic multicentric Castleman disease (iMCD) is a subtype of Castleman disease (also known as giant lymph node hyperplasia, lymphoid hamartoma, or angiofollicular lymph node hyperplasia), a group of lymphoproliferative disorders characterized by lymph node enlargement, characteristic features on microscopic analysis of enlarged lymph node tissue, and a range of symptoms and clinical findings.
The Castleman Disease Collaborative Network (CDCN) is an organization focused on research and awareness of Castleman disease. It was founded in 2012 and has used a collaborative network approach to advance several research studies on Castleman disease.
Epstein–Barr virus–associated lymphoproliferative diseases are a group of disorders in which one or more types of lymphoid cells, i.e. B cells, T cells, NK cells, and histiocytic-dendritic cells, are infected with the Epstein–Barr virus (EBV). This causes the infected cells to divide excessively, and is associated with the development of various non-cancerous, pre-cancerous, and cancerous lymphoproliferative disorders (LPDs). These LPDs include the well-known disorder occurring during the initial infection with the EBV, infectious mononucleosis, and the large number of subsequent disorders that may occur thereafter. The virus is usually involved in the development and/or progression of these LPDs although in some cases it may be an "innocent" bystander, i.e. present in, but not contributing to, the disease.