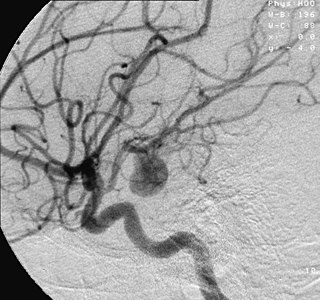
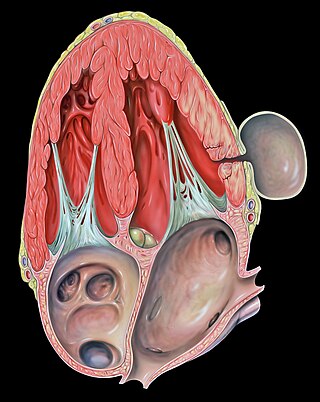
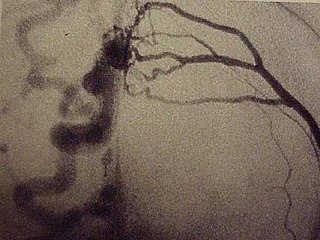
An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

A cerebral arteriovenous malformation is an abnormal connection between the arteries and veins in the brain—specifically, an arteriovenous malformation in the cerebrum.

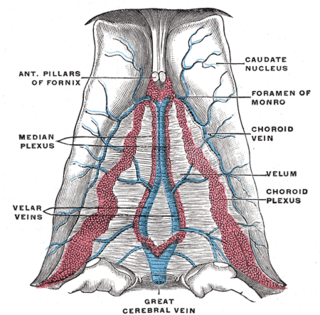
Veins are blood vessels in the circulatory system of humans and most other animals that carry blood toward the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

An intracranial aneurysm, also known as a cerebral aneurysm, is a cerebrovascular disorder in which weakness in the wall of a cerebral artery or vein causes a localized dilation or ballooning of the blood vessel.
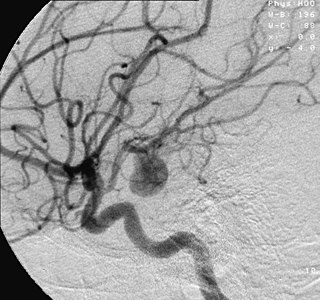
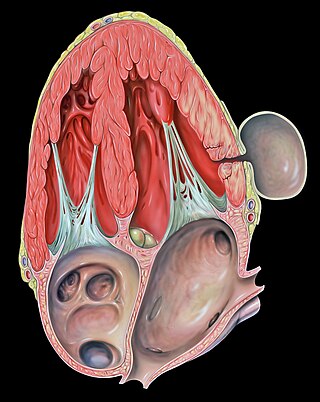
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus for clot formation (thrombosis) and embolization. As an aneurysm increases in size, the risk of rupture, which leads to uncontrolled bleeding, increases. Although they may occur in any blood vessel, particularly lethal examples include aneurysms of the Circle of Willis in the brain, aortic aneurysms affecting the thoracic aorta, and abdominal aortic aneurysms. Aneurysms can arise in the heart itself following a heart attack, including both ventricular and atrial septal aneurysms. There are congenital atrial septal aneurysms, a rare heart defect.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.
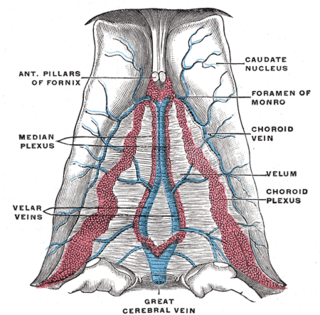
The great cerebral vein is one of the large blood vessels in the skull draining the cerebrum of the brain. It is also known as the vein of Galen, named for its discoverer, the Greek physician Galen.

Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.
A pseudoaneurysm, also known as a false aneurysm, is a locally contained hematoma outside an artery or the heart due to damage to the vessel wall. The injury passes through all three layers of the arterial wall, causing a leak, which is contained by a new, weak "wall" formed by the products of the clotting cascade. A pseudoaneurysm does not contain any layer of the vessel wall.

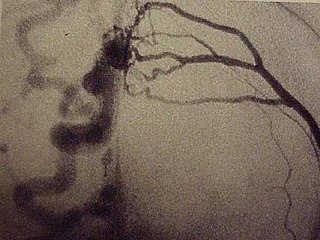
Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.

An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein. It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm.
An embolus, is described as a free-floating mass, located inside blood vessels that can travel from one site in the blood stream to another. An embolus can be made up of solid, liquid, or gas. Once these masses get "stuck" in a different blood vessel, it is then known as an "embolism." An embolism can cause ischemia—damage to an organ from lack of oxygen. A paradoxical embolism is a specific type of embolism in which the embolus travels from the right side of the heart to the left side of the heart and lodges itself in a blood vessel known as an artery. Thus, it is termed "paradoxical" because the embolus lands in an artery, rather than a vein.
The superior petrosal sinus is one of the dural venous sinuses located beneath the brain. It receives blood from the cavernous sinus and passes backward and laterally to drain into the transverse sinus. The sinus receives superior petrosal veins, some cerebellar veins, some inferior cerebral veins, and veins from the tympanic cavity. They may be affected by arteriovenous malformation or arteriovenous fistula, usually treated with surgery.
A dural arteriovenous fistula (DAVF) or malformation is an abnormal direct connection (fistula) between a meningeal artery and a meningeal vein or dural venous sinus.
A vascular malformation is a blood vessel or lymph vessel abnormality. Vascular malformations are one of the classifications of vascular anomalies, the other grouping is vascular tumors. They may cause aesthetic problems as they have a growth cycle, and can continue to grow throughout life.
Vascular myelopathy refers to an abnormality of the spinal cord in regard to its blood supply. The blood supply is complicated and supplied by two major vessel groups: the posterior spinal arteries and the anterior spinal arteries—of which the Artery of Adamkiewicz is the largest. Both the posterior and anterior spinal arteries run the entire length of the spinal cord and receive anastomotic (conjoined) vessels in many places. The anterior spinal artery has a less efficient supply of blood and is therefore more susceptible to vascular disease. Whilst atherosclerosis of spinal arteries is rare, necrosis in the anterior artery can be caused by disease in vessels originating from the segmental arteries such as atheroma or aortic dissection.

Bonnet–Dechaume–Blanc syndrome, also known as Wyburn-Mason syndrome, is a rare congenital disorder characterized by arteriovenous malformations of the brain, retina or facial nevi. The syndrome has a number of possible symptoms and can, more rarely, affect the skin, bones, kidneys, muscles, and gastrointestinal tract. When the syndrome affects the brain, people can experience severe headaches, seizures, acute stroke, meningism, and progressive neurological deficits due to acute or chronic ischaemia caused by arteriovenous shunting.
Interventional neuroradiology (INR) also known as neurointerventional surgery (NIS), endovascular therapy (EVT), endovascular neurosurgery, and interventional neurology is a medical subspecialty of neurosurgery, neuroradiology, intervention radiology and neurology specializing in minimally invasive image-based technologies and procedures used in diagnosis and treatment of diseases of the head, neck, and spine.
Alexander Coon is an American neurosurgeon who is the Director of Endovascular and Cerebrovascular Neurosurgery at the Carondelet Neurological Institute of St. Joseph's and St. Mary's Hospitals in Tucson, Arizona. He was previously the Director of Endovascular Neurosurgery at the Johns Hopkins Hospital and an assistant professor of neurosurgery, Neurology, and Radiology at the Johns Hopkins Hospital. He is known for his work in cerebrovascular and endovascular neurosurgery and his research in neuroendovascular devices and clinical outcomes in the treatment of cerebral aneurysms, subarachnoid hemorrhage, and AVMs.