Related Research Articles

Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.

Colpocephaly is a cephalic disorder involving the disproportionate enlargement of the occipital horns of the lateral ventricles and is usually diagnosed early after birth due to seizures. It is a nonspecific finding and is associated with multiple neurological syndromes, including agenesis of the corpus callosum, Chiari malformation, lissencephaly, and microcephaly. Although the exact cause of colpocephaly is not known yet, it is commonly believed to occur as a result of neuronal migration disorders during early brain development, intrauterine disturbances, perinatal injuries, and other central nervous system disorders. Individuals with colpocephaly have various degrees of motor disabilities, visual defects, spasticity, and moderate to severe intellectual disability. No specific treatment for colpocephaly exists, but patients may undergo certain treatments to improve their motor function or intellectual disability.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. This equals to 9–20 cmH2O, which is a common scale used in lumbar punctures. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.

A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from rips in bridging veins that cross the subdural space.

Cerebral circulation is the movement of blood through a network of cerebral arteries and veins supplying the brain. The rate of cerebral blood flow in an adult human is typically 750 milliliters per minute, or about 15% of cardiac output. Arteries deliver oxygenated blood, glucose and other nutrients to the brain. Veins carry "used or spent" blood back to the heart, to remove carbon dioxide, lactic acid, and other metabolic products. The neurovascular unit regulates cerebral blood flow so that activated neurons can be supplied with energy in the right amount and at the right time. Because the brain would quickly suffer damage from any stoppage in blood supply, the cerebral circulatory system has safeguards including autoregulation of the blood vessels. The failure of these safeguards may result in a stroke. The volume of blood in circulation is called the cerebral blood flow. Sudden intense accelerations change the gravitational forces perceived by bodies and can severely impair cerebral circulation and normal functions to the point of becoming serious life-threatening conditions.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Intraparenchymal hemorrhage is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage).
Vertebrobasilar insufficiency (VBI) describes a temporary set of symptoms due to decreased blood flow (ischemia) in the posterior circulation of the brain. The posterior circulation supplies the medulla, pons, midbrain, cerebellum and supplies the posterior cerebellar artery to the thalamus and occipital cortex. As a result, symptoms vary widely depending which brain region is predominantly affected.

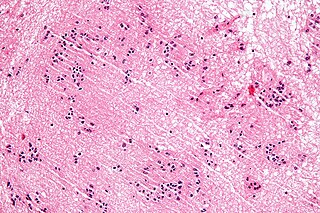
A tuberculoma is a clinical manifestation of tuberculosis which conglomerates tubercles into a firm lump, and so can mimic cancer tumors of many types in medical imaging studies. They often arise within individuals in whom a primary tuberculosis infection is not well controlled. When tuberculomas arise intracranially, they represent a manifestation of CNS tuberculosis. Since these are evolutions of primary complex, the tuberculomas may contain caseum or calcifications.
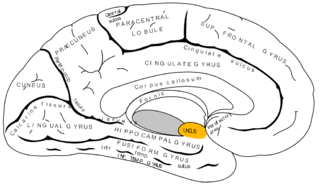
The uncus is an anterior extremity of the parahippocampal gyrus. It is separated from the apex of the temporal lobe by a sulcus called the rhinal sulcus. Although superficially continuous with the hippocampal gyrus, the uncus forms morphologically a part of the rhinencephalon.

Osmotherapy is the use of osmotically active substances to reduce the volume of intracranial contents. Osmotherapy serves as the primary medical treatment for cerebral edema. The primary purpose of osmotherapy is to improve elasticity and decrease intracranial volume by removing free water, accumulated as a result of cerebral edema, from brain's extracellular and intracellular space into vascular compartment by creating an osmotic gradient between the blood and brain. Normal serum osmolality ranges from 280 to 290 mOsm/kg and serum osmolality to cause water removal from brain without much side effects ranges from 300 to 320 mOsm/kg. Usually, 90 mL of space is created in the intracranial vault by 1.6% reduction in brain water content. Osmotherapy has cerebral dehydrating effects. The main goal of osmotherapy is to decrease intracranial pressure (ICP) by shifting excess fluid from brain. This is accomplished by intravenous administration of osmotic agents which increase serum osmolality in order to shift excess fluid from intracellular or extracellular space of the brain to intravascular compartment. The resulting brain shrinkage effectively reduces intracranial volume and decreases ICP.
A subependymoma is a type of brain tumor; specifically, it is a rare form of ependymal tumor. They are usually in middle aged people. Earlier, they were called subependymal astrocytomas.

Bonnet–Dechaume–Blanc syndrome, also known as Wyburn-Mason syndrome, is a rare congenital disorder characterized by arteriovenous malformations of the brain, retina or facial nevi. The syndrome has a number of possible symptoms and can, more rarely, affect the skin, bones, kidneys, muscles, and gastrointestinal tract. When the syndrome affects the brain, people can experience severe headaches, seizures, acute stroke, meningism, and progressive neurological deficits due to acute or chronic ischaemia caused by arteriovenous shunting.

An MRI pulse sequence in magnetic resonance imaging (MRI) is a particular setting of pulse sequences and pulsed field gradients, resulting in a particular image appearance.
Fogging phenomenon in computerized tomography (CT) scanning of the head is vanishing signs of an infarct on the serial CT imaging in a patient with a recent stroke. It is a reversal of the hypodensity on the CT after an acute ischemic stroke. This happens as a result of re-nourishment of the infarcted area in subacute phase about one to three weeks after the stroke. In fact, resolution of the edema, which was caused by the accident, leads to increased attenuation of infarcted area that may regain near-normal density and mask the stroke. However, in the third week, parenchymal volume loss commonly appears as a hypoattenuation with a negative mass effect (shrinkage).
A pseudosubarachnoid hemorrhage is an apparent increased attenuation on CT scans within the basal cisterns that mimics a true subarachnoid hemorrhage. This occurs in cases of severe cerebral edema, such as by cerebral hypoxia. It may also occur due to intrathecally administered contrast material, leakage of high-dose intravenous contrast material into the subarachnoid spaces, or in patients with cerebral venous sinus thrombosis, severe meningitis, leptomeningeal carcinomatosis, intracranial hypotension, cerebellar infarctions, or bilateral subdural hematomas.
References
- ↑ Chavhan, GB; Shroff, MM (2008). "Twenty classic signs in neuroradiology: A pictorial essay". The Indian Journal of Radiology & Imaging. 19 (2): 135–45. doi: 10.4103/0971-3026.50835 . PMC 2765171 . PMID 19881070.
- 1 2 3 Chalela, JA; Rothlisberger, J; West, B; Hays, A (June 2013). "The white cerebellum sign: an under recognized sign of increased intracranial pressure". Neurocritical Care. 18 (3): 398–9. doi:10.1007/s12028-013-9836-z. PMID 23589182. S2CID 2152985.
- ↑ Han, BK; Towbin, RB; De Courten-Myers, G; McLaurin, RL; Ball WS, Jr (1988). "Reversal sign on CT: effect of anoxic/ischemic cerebral injury in children". AJNR. American Journal of Neuroradiology. 10 (6): 1191–8. PMC 8332434 . PMID 2512781.
- ↑ Krishnan, P; Chowdhury, SR (October 2014). ""White cerebellum" sign - A dark prognosticator". Journal of Neurosciences in Rural Practice. 5 (4): 433. doi: 10.4103/0976-3147.140015 . PMC 4173255 . PMID 25288860.