Cartilage is a resilient and smooth type of connective tissue. It is a semi-transparent and non-porous type of tissue. It is usually covered by a tough and fibrous membrane called perichondrium. In tetrapods, it covers and protects the ends of long bones at the joints as articular cartilage, and is a structural component of many body parts including the rib cage, the neck and the bronchial tubes, and the intervertebral discs. In other taxa, such as chondrichthyans, but also in cyclostomes, it may constitute a much greater proportion of the skeleton. It is not as hard and rigid as bone, but it is much stiffer and much less flexible than muscle. The matrix of cartilage is made up of glycosaminoglycans, proteoglycans, collagen fibers and, sometimes, elastin. It usually grows quicker than bone.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
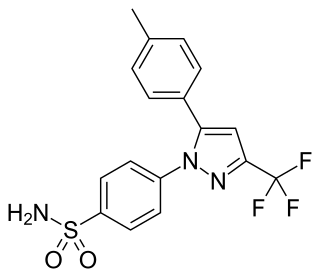
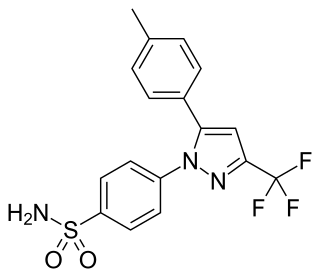
Celecoxib, sold under the brand name Celebrex among others, is a COX-2 inhibitor and nonsteroidal anti-inflammatory drug (NSAID). It is used to treat the pain and inflammation in osteoarthritis, acute pain in adults, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, painful menstruation, and juvenile rheumatoid arthritis. It may also be used to decrease the risk of colorectal adenomas in people with familial adenomatous polyposis. It is taken by mouth. Benefits are typically seen within an hour.
Glucosamine (C6H13NO5) is an amino sugar and a prominent precursor in the biochemical synthesis of glycosylated proteins and lipids. Glucosamine is part of the structure of two polysaccharides, chitosan and chitin. Glucosamine is one of the most abundant monosaccharides. Produced commercially by the hydrolysis of shellfish exoskeletons or, less commonly, by fermentation of a grain such as corn or wheat, glucosamine has many names depending on country.

Dimethyl sulfone (DMSO2) is an organosulfur compound with the formula (CH3)2SO2. It is also known by several other names including methyl sulfone and (especially in alternative medicine) methylsulfonylmethane (MSM). This colorless solid features the sulfonyl functional group and is the simplest of the sulfones. It is relatively inert chemically and is able to resist decomposition at elevated temperatures. It occurs naturally in some primitive plants, is present in small amounts in many foods and beverages, and is marketed (under the MSM name) as a dietary supplement. It is sometimes used as a cutting agent for illicitly manufactured methamphetamine. It is also commonly found in the atmosphere above marine areas, where it is used as a carbon source by the airborne bacteria Afipia. Oxidation of dimethyl sulfoxide produces the sulfone, both under laboratory conditions and metabolically.
A chondroitin is a chondrin derivative.

In medicine, a joint injection is a procedure used in the treatment of inflammatory joint conditions, such as rheumatoid arthritis, psoriatic arthritis, gout, tendinitis, bursitis, Carpal Tunnel Syndrome, and occasionally osteoarthritis. A hypodermic needle is injected into the affected joint where it delivers a dose of any one of many anti-inflammatory agents, the most common of which are corticosteroids. Hyaluronic acid, because of its high viscosity, is sometimes used to replace bursa fluids. The technique may be used to also withdraw excess fluid from the joint.

Pentosan polysulfate, sold under the brand name Elmiron among others, is a medication used for the treatment of interstitial cystitis. It was approved for medical use in the United States in 1996.
Chondropathy refers to a disease of the cartilage. It is frequently divided into 5 grades, with 0-2 defined as normal and 3-4 defined as diseased.
Heparinoids are glycosaminoglycans which are chemically and pharmacologically related to heparin. They include oligosaccharides and sulfated polysaccharides of plant, animal, or synthetic origin. Multiple scientific studies have been conducted on heparinoids.
Naproxcinod (nitronaproxen) is a nonsteroidal anti-inflammatory drug (NSAID) developed by the French pharmaceutical company NicOx. It is a derivative of naproxen with a nitroxybutyl ester to allow it to also act as a nitric oxide (NO) donor. This second mechanism of action makes naproxcinod the first in a new class of drugs, the cyclooxygenase inhibiting nitric oxide donators (CINODs), that are hoped to produce similar analgesic efficacy to traditional NSAIDs, but with less gastrointestinal and cardiovascular side effects.
Tanezumab is a monoclonal antibody against nerve growth factor as a treatment for pain via a novel mechanisms different from conventional pain-killer drugs. Tanezumab was discovered and developed by Rinat Neuroscience and was acquired by Pfizer in 2006.

Sodium hyaluronate is the sodium salt of hyaluronic acid, a glycosaminoglycan found in various connective tissue of humans.

Arthritis of the knee is typically a particularly debilitating form of arthritis. The knee may become affected by almost any form of arthritis.
Cosequin is a nutritional supplement for animals. It claims to support joints in pets.
Celadrin is an over-the-counter medication marketed as a topical analgesic. It is a cream that is used for muscle and joint pains including osteoarthritis, strains, bruises, and sprains. The active ingredient is menthol and it also contains cetylated and esterified fatty acids. The inactive ingredients are Benzyl Alcohol, Butylparaben, carbomer interpolymer type a, ethylparaben, glycerin, glyceryl monostearate, isobutylparaben, soybean, methylparaben, olive oil, PEG-100 Stearate, peppermint oil, phenoxyethanol, sodium hydroxide, propylparaben, alpha-tocopherol acetate, and water.
A significant amount of research has been performed on glycosaminoglycans, especially glucosamine and chondroitin, for the treatment of arthritis. These compounds are commonly marketed as nutritional supplements and numerous 'soft therapeutic claims' are made about their health benefits - especially in aging populations. Since glucosamine is a precursor for glycosaminoglycans, and glycosaminoglycans are major components of cartilage, ingesting glucosamine might nourish joints, and thereby alleviate arthritis symptoms. Authoritative opinions on the actual therapeutic value of these compounds have been very mixed.
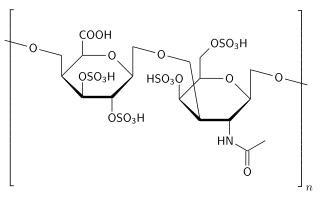
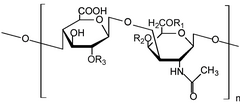
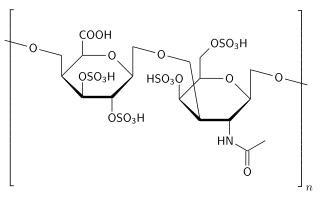
Polysulfated glycosaminoglycan (PSGAG), sold under the brand name Adequan, is an injectable drug for dogs and horses that is used to alleviate the limpness, pain, and lowered range of motion caused by arthritis. It is made of repeat disaccharide units (comprising hexosamine and hexuronic acid), and is similar to glycosaminoglycans already present in the cartilage; PSGAG thus easily integrates itself there. In vitro studies have shown it to inhibit the enzymes that degrade cartilage and bone, as well as suppress inflammation and stimulate the synthesis of replacement cartilage. While it can cause an increased risk of bleeding, it is relatively safe and has a high LD50. PSGAG is one of the most widely prescribed joint treatments for horses.

Senior dog food diets are pet foods that are catered toward the senior or mature pet population. The senior dog population consists of dogs that are over the age of seven for most dog breeds, though in general large and giant breed dogs tend to reach this life stage earlier when compared to smaller breed dogs. Senior dog foods contain nutrients and characteristics that are used to improve the health of the aging dog. Aging in dogs causes many changes to occur physiologically that will require a change in nutrient composition of their diet.
A disease-modifying osteoarthritis drug (DMOAD) is a disease-modifying drug that would inhibit or even reverse the progression of osteoarthritis. Since the main hallmark of osteoarthritis is cartilage loss, a typical DMOAD would prevent the loss of cartilage and potentially regenerate it. Other DMOADs may attempt to help repair adjacent tissues by reducing inflammation. A successful DMOAD would be expected to show an improvement in patient pain and function with an improvement of the health of the joint tissues.