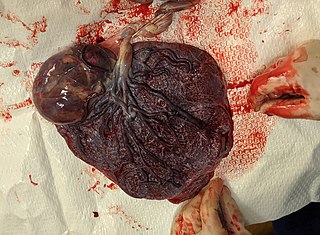
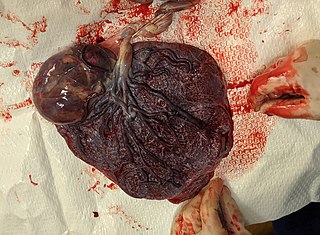
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

Placental mammals are one of the three extant subdivisions of the class Mammalia, the other two being Monotremata and Marsupialia. Placentalia contains the vast majority of extant mammals, which are partly distinguished from monotremes and marsupials in that the fetus is carried in the uterus of its mother to a relatively late stage of development. The name is something of a misnomer considering that marsupials also nourish their fetuses via a placenta, though for a relatively briefer period, giving birth to less developed young which are then nurtured for a period inside the mother's pouch.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.

The trophoblast is the outer layer of cells of the blastocyst. Trophoblasts are present four days after fertilization in humans. They provide nutrients to the embryo and develop into a large part of the placenta. They form during the first stage of pregnancy and are the first cells to differentiate from the fertilized egg to become extraembryonic structures that do not directly contribute to the embryo. After blastulation, the trophoblast is contiguous with the ectoderm of the embryo and is referred to as the trophectoderm. After the first differentiation, the cells in the human embryo lose their totipotency because they can no longer form a trophoblast. They become pluripotent stem cells.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.

The decidua is the modified mucosal lining of the uterus that forms every month, in preparation for pregnancy. It is shed off each month when there is no fertilised egg to support. The decidua is under the influence of progesterone. Endometrial cells become highly characteristic. The decidua forms the maternal part of the placenta and remains for the duration of the pregnancy. After birth the decidua is shed together with the placenta.

Placentation refers to the formation, type and structure, or arrangement of the placenta. The function of placentation is to transfer nutrients, respiratory gases, and water from maternal tissue to a growing embryo, and in some instances to remove waste from the embryo. Placentation is best known in live-bearing mammals (theria), but also occurs in some fish, reptiles, amphibians, a diversity of invertebrates, and flowering plants. In vertebrates, placentas have evolved more than 100 times independently, with the majority of these instances occurring in squamate reptiles.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

Placental growth factor(PlGF) is a protein that in humans is encoded by the PGF gene.

A placental disease is any disease, disorder, or pathology of the placenta.
Post-maturity syndrome develops in about 20% of human pregnancies continuing past the expected dates. Ten years ago it was generally held that the postmature fetus ran some risk of dying in the uterus before the onset of labour because of degeneration and calcification of the placenta. Features of post-maturity syndrome include oligohydramnios, meconium aspiration, macrosomia and fetal problems such as dry peeling skin, overgrown nails, abundant scalp hair, visible creases on palms and soles, minimal fat deposition and skin colour become green or yellow due to meconium staining. Post-maturity refers to any baby born after 42 weeks gestation or 294 days past the first day of the mother's last menstrual period. Less than 6 percent of all babies are born at 42 weeks or later. In most cases, continued fetal growth between 39 and 43 wk gestation results in a macrosomic infant. However, sometimes the placenta involutes, and multiple infarcts and villous degeneration cause placental insufficiency syndrome. In this syndrome, the fetus receives inadequate nutrients and oxygen from the mother, resulting in a thin, small-for-gestational-age, undernourished infant with depleted glycogen stores. Post term, the amniotic fluid volume eventually decreases, leading to oligohydramnios. Although pregnancy is said to last nine months, health care providers track pregnancy by weeks and days. The estimated delivery date, also called the estimated due date or EDD, is calculated as 40 weeks or 280 days from the first day of the last menstrual period. Only 4 percent women will deliver on their due date. The terms Post-maturity or "Post-term" are both words used to describe babies born after 42 weeks. The terms "post-maturity" and "post-term" are interchangeable. As there are many definitions for prolonged pregnancy the incidence varies from 2 to 10%. When incidence is taken as delivery beyond 42 weeks it is 10%, if it is taken according to the delivered baby's weight and length it is 2%. The baby may have birth weight of 4 kg and length of 54 cm but these findings are variable, even the baby may have underweight. Post-maturity is more likely to happen when a mother has had a post-term pregnancy before. After one post-term pregnancy, the risk of a second post-term birth increases by 2 to 3 times. Other, minor risk factors include an older or obese mother, a white mother, male baby, or a family history of post-maturity. Maternal risks include obstructed labor, perennial damage, instrumental vaginal delivery, a Cesarean section, infection, and post postpartum hemorrhage. Accurate pregnancy due dates can help identify babies at risk for post-maturity. Ultrasound examinations early in pregnancy help establish more accurate dating by measurements taken of the fetus. Pregnancies complicated by gestational diabetes, hypertension, or other high-risk conditions should be managed according to guidelines for those conditions.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
Birth injury refers to damage or injury to the child before, during, or just after the birthing process. "Birth trauma" refers specifically to mechanical damage sustained during delivery.

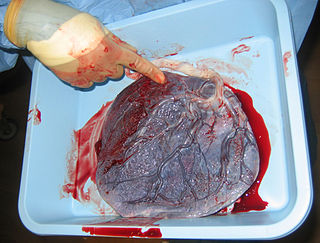
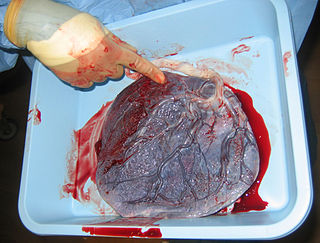
Placental expulsion occurs when the placenta comes out of the birth canal after childbirth. The period from just after the baby is expelled until just after the placenta is expelled is called the third stage of labor.

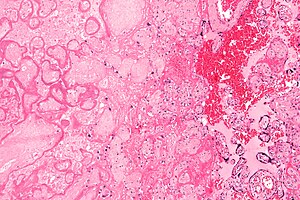
Villitis of unknown etiology (VUE), also known as chronic villitis, is a placental injury. VUE is an inflammatory condition involving the chorionic villi. VUE is a recurrent condition and can be associated with intrauterine growth restriction (IUGR). IUGR involves the poor growth of the foetus, stillbirth, miscarriage, and premature delivery. VUE recurs in about 1/3 of subsequent pregnancies.
Chorioangioma, or chorangioma, is a benign tumor of placenta. It is a hamartoma-like growth in the placenta consisting of blood vessels, and is seen in approximately 0.5 to 1% pregnancies. It is mostly diagnosed ultrasonically in the second trimester of pregnancy. Large chorioangiomas are known to cause complications in pregnancy, while the smaller ones are asymptomatic.
Breus' mole is a massive, subchorionic, tuberous hematoma formed from maternal blood in the uterus during pregnancy. It was first described by Karl Breus in 1892.
Raissa Nitabuch was a Russian Empire pathologist who is known for her histological studies of the human placenta. The layer of fibrin that was thought to separate the uterine decidua from the fetoplacental trophoblast after birth was named the Nitabuch layer or Nitabuch membrane, thus becoming the only woman whose name is "affiliated with a macroscopic anatomical structure."
Massive perivillous fibrin deposition refers to excessive deposition of fibrous tissue around the chorionic villi of the placenta. It causes reduced growth of the foetus, and leads to miscarriage in nearly 1 in 3 pregnancies affected. There are typically no symptoms, and it is rarely detected before birth. The cause is unknown, but may be autoimmune. Diagnosis is based on the histology of the placenta. There are currently no known treatments. MPFD is very rare, but recurrence is around 18% in those affected.