Locked-in syndrome (LIS), also known as pseudocoma, is a condition in which a patient is aware but cannot move or communicate verbally due to complete paralysis of nearly all voluntary muscles in the body except for vertical eye movements and blinking. The individual is conscious and sufficiently intact cognitively to be able to communicate with eye movements. Electroencephalography results are normal in locked-in syndrome. Total locked-in syndrome, or completely locked-in state (CLIS), is a version of locked-in syndrome wherein the eyes are paralyzed as well. Fred Plum and Jerome B. Posner coined the term for this disorder in 1966.

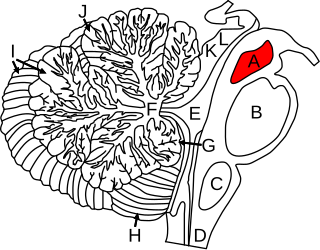
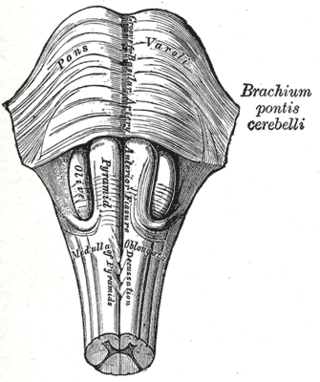
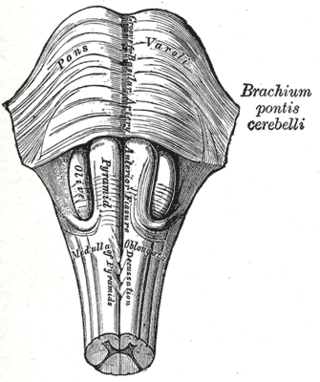
The pons is part of the brainstem that in humans and other mammals lies inferior to the midbrain, superior to the medulla oblongata and anterior to the cerebellum.

The brainstem is the stalk-like part of the brain that interconnects the cerebrum and diencephalon with the spinal cord. In the human brain, the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is continuous with the thalamus of the diencephalon through the tentorial notch.
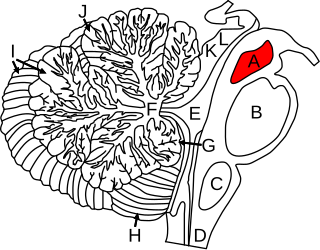
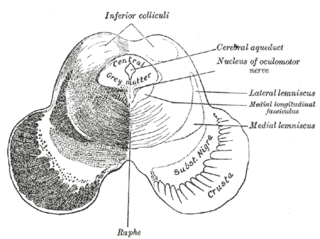
The midbrain or mesencephalon is the rostral-most portion of the brainstem connecting the diencephalon and cerebrum with the pons. It consists of the cerebral peduncles, tegmentum, and tectum.

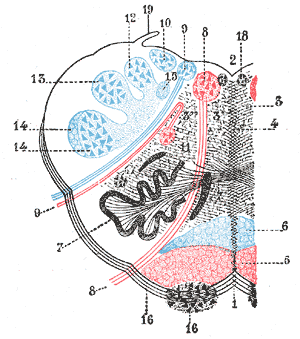
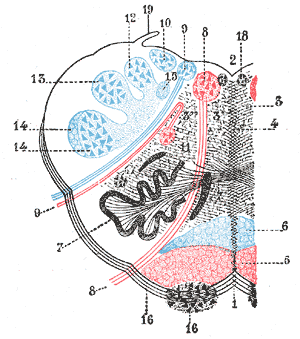
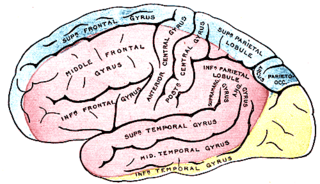
The internal capsule is a white matter structure situated in the inferomedial part of each cerebral hemisphere of the brain. It carries information past the basal ganglia, separating the caudate nucleus and the thalamus from the putamen and the globus pallidus. The internal capsule contains both ascending and descending axons, going to and coming from the cerebral cortex. It also separates the caudate nucleus and the putamen in the dorsal striatum, a brain region involved in motor and reward pathways.
Lateral medullary syndrome is a neurological disorder causing a range of symptoms due to ischemia in the lateral part of the medulla oblongata in the brainstem. The ischemia is a result of a blockage most commonly in the vertebral artery or the posterior inferior cerebellar artery. Lateral medullary syndrome is also called Wallenberg's syndrome, posterior inferior cerebellar artery (PICA) syndrome and vertebral artery syndrome.
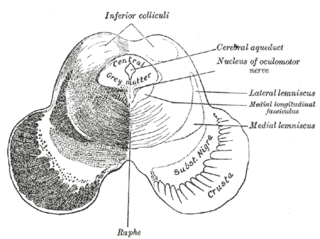
The medial longitudinal fasciculus (MLF) is an area of crossed over tracts, on each side of the brainstem. These bundles of axons are situated near the midline of the brainstem. They are made up of both ascending and descending fibers that arise from a number of sources and terminate in different areas, including the superior colliculus, the vestibular nuclei, and the cerebellum. It contains the interstitial nucleus of Cajal, responsible for oculomotor control, head posture, and vertical eye movement.
Medial medullary syndrome, also known as inferior alternating syndrome, hypoglossal alternating hemiplegia, lower alternating hemiplegia, or Dejerine syndrome, is a type of alternating hemiplegia characterized by a set of clinical features resulting from occlusion of the anterior spinal artery. This results in the infarction of medial part of the medulla oblongata.

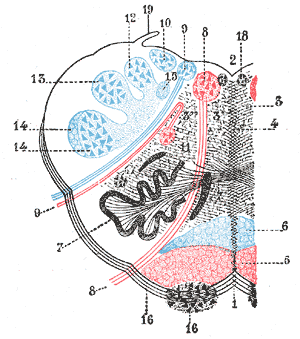
The reticular formation is a set of interconnected nuclei that are located throughout the brainstem. It is not anatomically well defined, because it includes neurons located in different parts of the brain. The neurons of the reticular formation make up a complex set of networks in the core of the brainstem that extend from the upper part of the midbrain to the lower part of the medulla oblongata. The reticular formation includes ascending pathways to the cortex in the ascending reticular activating system (ARAS) and descending pathways to the spinal cord via the reticulospinal tracts.

Jean-Dominique Bauby was a French journalist, author and editor of the French fashion magazine Elle.
Abnormal posturing is an involuntary flexion or extension of the arms and legs, indicating severe brain injury. It occurs when one set of muscles becomes incapacitated while the opposing set is not, and an external stimulus such as pain causes the working set of muscles to contract. The posturing may also occur without a stimulus. Since posturing is an important indicator of the amount of damage that has occurred to the brain, it is used by medical professionals to measure the severity of a coma with the Glasgow Coma Scale and the Pediatric Glasgow Coma Scale.
The posterior cerebral artery (PCA) is one of a pair of cerebral arteries that supply oxygenated blood to the occipital lobe, part of the back of the human brain. The two arteries originate from the distal end of the basilar artery, where it bifurcates into the left and right posterior cerebral arteries. These anastomose with the middle cerebral arteries and internal carotid arteries via the posterior communicating arteries.

The nucleus of the trochlear nerve is a motor nucleus in the medial midbrain giving rise to the trochlear nerve.

Weber's syndrome, also known as midbrain stroke syndrome or superior alternating hemiplegia, is a form of stroke that affects the medial portion of the midbrain. It involves oculomotor fascicles in the interpeduncular cisterns and cerebral peduncle so it characterizes the presence of an ipsilateral lower motor neuron type oculomotor nerve palsy and contralateral hemiparesis or hemiplegia.

Medial inferior pontine syndrome is a condition associated with a contralateral hemiplegia."Medial inferior pontine syndrome" has been described as equivalent to Foville's syndrome.

A lateral pontine syndrome is a lesion which is similar to the lateral medullary syndrome, but because it occurs in the pons, it also involves the cranial nerve nuclei of the pons.
Claude's syndrome is a form of brainstem stroke syndrome characterized by the presence of an ipsilateral oculomotor nerve palsy, contralateral hemiparesis, contralateral ataxia, and contralateral hemiplegia of the lower face, tongue, and shoulder. Claude's syndrome affects oculomotor nerve, red nucleus and brachium conjunctivum.
Babinski–Nageotte syndrome is an alternating brainstem syndrome. It occurs when there is damage to the dorsolateral or posterior lateral medulla oblongata, likely syphilitic in origin. Hence it is also called the alternating medulla oblongata syndrome.
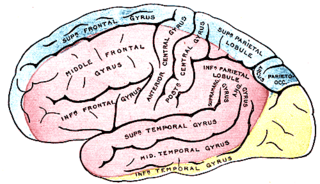
Alternating hemiplegia is a form of hemiplegia that has an ipsilateral cranial nerve palsies and contralateral hemiplegia or hemiparesis of extremities of the body. The disorder is characterized by recurrent episodes of paralysis on one side of the body. There are multiple forms of alternating hemiplegia, Weber's syndrome, middle alternating hemiplegia, and inferior alternating hemiplegia. This type of syndrome can result from a unilateral lesion in the brainstem affecting both upper motor neurons and lower motor neurons. The muscles that would receive signals from these damaged upper motor neurons result in spastic paralysis. With a lesion in the brainstem, this affects the majority of limb and trunk muscles on the contralateral side due to the upper motor neurons decussation after the brainstem. The cranial nerves and cranial nerve nuclei are also located in the brainstem making them susceptible to damage from a brainstem lesion. Cranial nerves III (Oculomotor), VI (Abducens), and XII (Hypoglossal) are most often associated with this syndrome given their close proximity with the pyramidal tract, the location which upper motor neurons are in on their way to the spinal cord. Damages to these structures produce the ipsilateral presentation of paralysis or palsy due to the lack of cranial nerve decussation before innervating their target muscles. The paralysis may be brief or it may last for several days, many times the episodes will resolve after sleep. Some common symptoms of alternating hemiplegia are mental impairment, gait and balance difficulties, excessive sweating and changes in body temperature.