Related Research Articles

Antiviral drugs are a class of medication used for treating viral infections. Most antivirals target specific viruses, while a broad-spectrum antiviral is effective against a wide range of viruses. Antiviral drugs are one class of antimicrobials, a larger group which also includes antibiotic, antifungal and antiparasitic drugs, or antiviral drugs based on monoclonal antibodies. Most antivirals are considered relatively harmless to the host, and therefore can be used to treat infections. They should be distinguished from virucides, which are not medication but deactivate or destroy virus particles, either inside or outside the body. Natural virucides are produced by some plants such as eucalyptus and Australian tea trees.
An HIV vaccine is a potential vaccine that could be either a preventive vaccine or a therapeutic vaccine, which means it would either protect individuals from being infected with HIV or treat HIV-infected individuals.
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.
The spread of HIV/AIDS has affected millions of people worldwide; AIDS is considered a pandemic. The World Health Organization (WHO) estimated that in 2016 there were 36.7 million people worldwide living with HIV/AIDS, with 1.8 million new HIV infections per year and 1 million deaths due to AIDS. Misconceptions about HIV and AIDS arise from several different sources, from simple ignorance and misunderstandings about scientific knowledge regarding HIV infections and the cause of AIDS to misinformation propagated by individuals and groups with ideological stances that deny a causative relationship between HIV infection and the development of AIDS. Below is a list and explanations of some common misconceptions and their rebuttals.
The National Institute of Allergy and Infectious Diseases is one of the 27 institutes and centers that make up the National Institutes of Health (NIH), an agency of the United States Department of Health and Human Services (HHS). NIAID's mission is to conduct basic and applied research to better understand, treat, and prevent infectious, immunologic, and allergic diseases.
This is a list of AIDS-related topics, many of which were originally taken from the public domain U.S. Department of Health Glossary of HIV/AIDS-Related Terms, 4th Edition.

The AIDS Clinical Trials Group network (ACTG) is one of the largest HIV clinical trials organizations in the world, playing a major role in setting standards of care for HIV infection and opportunistic diseases related to HIV and AIDS in the United States and the developing world. The ACTG is composed of, and directed by, leading clinical scientists in HIV/AIDS therapeutic research. The ACTG is funded by the Department of Health and Human Services, National Institutes of Health through the National Institute of Allergy and Infectious Diseases.

Infection with HIV, a retrovirus, can be managed with treatment but without treatment can lead to a spectrum of conditions including AIDS.
Douglas D. Richman is an American infectious diseases physician and medical virologist. Richman's work has focused on the HIV/AIDS pandemic, since its appearance in the early 1980s. His major contributions have been in the areas of treatment, drug resistance, and pathogenicity.

The HIV Prevention Trials Network (HPTN) is a worldwide collaborative clinical trials network that brings together investigators, ethicists, community and other partners to develop and test the safety and efficacy of interventions designed to prevent the acquisition and transmission of HIV. HPTN studies evaluate new HIV prevention interventions and strategies in populations and geographical regions that bear a disproportionate burden of infection. The HPTN is committed to the highest ethical standards for its clinical trials and recognizes the importance of community engagement in all phases of the research process.
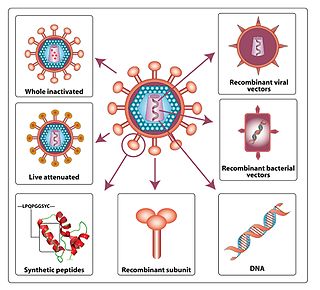
GeoVax is a clinical-stage biotechnology company which develops vaccines. GeoVax’s development platform uses Modified Vaccinia Ankara (MVA) vector technology, with improvements to antigen design and manufacturing capabilities. GeoVax uses recombinant DNA or recombinant viruses to produce virus-like particles (VLPs) in the person being vaccinated.

The Vaccine Research Center (VRC), is an intramural division of the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), US Department of Health and Human Services (HHS). The mission of the VRC is to discover and develop both vaccines and antibody-based products that target infectious diseases.
The United States Military HIV Research Program was initiated by the United States Congress in 1986, in reaction to the threat of lost effectiveness of U.S./Allied troops due to HIV infection. The mission of MHRP is to develop an HIV-1 vaccine, provide prevention, care, and treatment, and conduct meaningful HIV/AIDS research for the global community through the President's Emergency Plan for AIDS Relief (PEPFAR). It is centered at the Walter Reed Army Institute of Research (WRAIR), and has established five international research sites in Africa and Asia. MHRP also partners with the Armed Forces Research Institute of Medical Sciences (AFRIMS) in Thailand. MHRP works closely with The Henry M. Jackson Foundation for the Advancement of Military Medicine (HJF), most notably in the development of the RV144 HIV vaccine in Thailand. MHRP is the largest research program supported by the HJF.

Jeffrey P. Nadler is an American Infectious Diseases and HIV/AIDS expert. His most recent position has been as Acting Director and Assistant Director of the Therapeutics Research Program, Division of AIDS (DAIDS), National Institute of Allergy and Infectious Diseases (NIAID) where he oversaw NIH/NIAID-sponsored national and international HIV/AIDS research.

HIV/AIDS research includes all medical research that attempts to prevent, treat, or cure HIV/AIDS, as well as fundamental research about the nature of HIV as an infectious agent and AIDS as the disease caused by HIV.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
Treatment as prevention (TasP) is a concept in public health that promotes treatment as a way to prevent and reduce the likelihood of HIV illness, death and transmission from an infected individual to others. Expanding access to earlier HIV diagnosis and treatment as a means to address the global epidemic by preventing illness, death and transmission was first proposed in 2000 by Garnett et al. The term is often used to talk about treating people that are currently living with human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) to prevent illness, death and transmission. Although some experts narrow this to only include preventing infections, treatment prevents illnesses such as tuberculosis and has been shown to prevent death. The dual impact on well-being and its 100% effectiveness in reducing transmission makes TasP the most important element in the HIV prevention toolkit. In relation to HIV, antiretroviral therapy (ART) is a three or more drug combination therapy that is used to decrease the viral load, or the measured amount of virus, in an infected individual. Such medications are used as a preventative for infected individuals to not only spread the HIV virus to their negative partners but also improve their current health to increase their lifespans. Other names for ART include highly active antiretroviral therapy (HAART), combination antiretroviral therapy (cART), triple therapy and triple drug cocktail. When taken correctly, ART is able to diminish the presence of the HIV virus in the bodily fluids of an infected person to a level of undetectability. Undetectability ensures that infection does not necessarily have an effect on a person's general health, and that there is no longer a risk of passing along HIV to others. Consistent adherence to an ARV regimen, monitoring, and testing are essential for continued confirmed viral suppression. Treatment as prevention rose to great prominence in 2011, as part of the HPTN 052 study, which shed light on the benefits of early treatment for HIV positive individuals.

Lauren V. Wood is an American allergist, immunologist, and staff physician at the National Cancer Institute (NCI) at the National Institutes of Health (NIH) in Bethesda, Maryland, where she has served as a principal investigator. She is known for conducting studies of vaccines for cancer, Human papillomavirus (HPV), Hepatitis C, and HIV especially for use with children, teens and young adults. She holds the rank of captain in the U.S. Public Health Service (PHS).
Viral load monitoring for HIV is the regular measurement of the viral load of individual HIV-positive people as part of their personal plan for treatment of HIV/AIDS. A count of the viral load is routine before the start of HIV treatment.
References
- ↑ "NOT-AI-09-053: RFP ANNOUNCEMENT: External Quality Assurance Program Oversight Laboratory (EQAPOL)". grants.nih.gov. Retrieved 2023-09-05.
