Related Research Articles
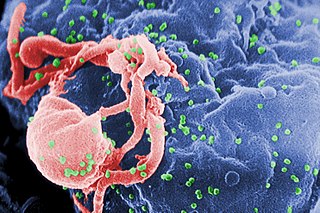
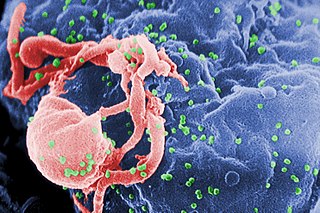
The human immunodeficiency viruses (HIV) are two species of Lentivirus that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive. Without treatment, the average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype.
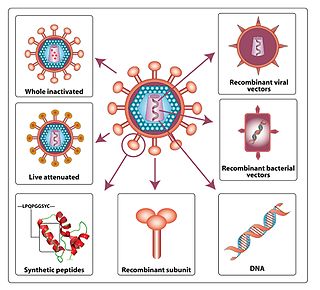
An HIV vaccine is a potential vaccine that could be either a preventive vaccine or a therapeutic vaccine, which means it would either protect individuals from being infected with HIV or treat HIV-infected individuals.
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.

A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular pathogens (such as viruses or bacteria), or cells that are damaged in other ways.

The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of T cell that play an important role in the adaptive immune system. They aid the activity of other immune cells by releasing cytokines. They are considered essential in B cell antibody class switching, breaking cross-tolerance in dendritic cells, in the activation and growth of cytotoxic T cells, and in maximizing bactericidal activity of phagocytes such as macrophages and neutrophils. CD4+ cells are mature Th cells that express the surface protein CD4. Genetic variation in regulatory elements expressed by CD4+ cells determines susceptibility to a broad class of autoimmune diseases.
The spread of HIV/AIDS has affected millions of people worldwide; AIDS is considered a pandemic. The World Health Organization (WHO) estimated that in 2016 there were 36.7 million people worldwide living with HIV/AIDS, with 1.8 million new HIV infections per year and 1 million deaths due to AIDS. Misconceptions about HIV and AIDS arise from several different sources, from simple ignorance and misunderstandings about scientific knowledge regarding HIV infections and the cause of AIDS to misinformation propagated by individuals and groups with ideological stances that deny a causative relationship between HIV infection and the development of AIDS. Below is a list and explanations of some common misconceptions and their rebuttals.

Simian immunodeficiency virus (SIV) is a species of retrovirus that cause persistent infections in at least 45 species of non-human primates. Based on analysis of strains found in four species of monkeys from Bioko Island, which was isolated from the mainland by rising sea levels about 11,000 years ago, it has been concluded that SIV has been present in monkeys and apes for at least 32,000 years, and probably much longer.

C-C chemokine receptor type 5, also known as CCR5 or CD195, is a protein on the surface of white blood cells that is involved in the immune system as it acts as a receptor for chemokines.
AIDS-defining clinical conditions is the list of diseases published by the Centers for Disease Control and Prevention (CDC) that are associated with AIDS and used worldwide as a guideline for AIDS diagnosis. CDC exclusively uses the term AIDS-defining clinical conditions, but the other terms remain in common use.

Envelope glycoprotein GP120 is a glycoprotein exposed on the surface of the HIV envelope. It was discovered by Professors Tun-Hou Lee and Myron "Max" Essex of the Harvard School of Public Health in 1984. The 120 in its name comes from its molecular weight of 120 kDa. Gp120 is essential for virus entry into cells as it plays a vital role in attachment to specific cell surface receptors. These receptors are DC-SIGN, Heparan Sulfate Proteoglycan and a specific interaction with the CD4 receptor, particularly on helper T-cells. Binding to CD4 induces the start of a cascade of conformational changes in gp120 and gp41 that lead to the fusion of the viral membrane with the host cell membrane. Binding to CD4 is mainly electrostatic although there are van der Waals interactions and hydrogen bonds.
HIV-associated neurocognitive disorders (HAND) are neurological disorders associated with HIV infection and AIDS. It is a syndrome of progressive deterioration of memory, cognition, behavior, and motor function in HIV-infected individuals during the late stages of the disease, when immunodeficiency is severe. HAND may include neurological disorders of various severity. HIV-associated neurocognitive disorders are associated with a metabolic encephalopathy induced by HIV infection and fueled by immune activation of macrophages and microglia. These cells are actively infected with HIV and secrete neurotoxins of both host and viral origin. The essential features of HIV-associated dementia (HAD) are disabling cognitive impairment accompanied by motor dysfunction, speech problems and behavioral change. Cognitive impairment is characterised by mental slowness, trouble with memory and poor concentration. Motor symptoms include a loss of fine motor control leading to clumsiness, poor balance and tremors. Behavioral changes may include apathy, lethargy and diminished emotional responses and spontaneity. Histopathologically, it is identified by the infiltration of monocytes and macrophages into the central nervous system (CNS), gliosis, pallor of myelin sheaths, abnormalities of dendritic processes and neuronal loss.
Entry inhibitors, also known as fusion inhibitors, are a class of antiviral drugs that prevent a virus from entering a cell, for example, by blocking a receptor. Entry inhibitors are used to treat conditions such as HIV and hepatitis D.
HIV superinfection is a condition in which a person with an established human immunodeficiency virus infection acquires a second strain of HIV, often of a different subtype. These can form a recombinant strain that co-exists with the strain from the initial infection, as well from reinfection with a new virus strain, and may cause more rapid disease progression or carry multiple resistances to certain HIV medications.
CD4 immunoadhesin is a recombinant fusion protein consisting of a combination of CD4 and the fragment crystallizable region, similarly known as immunoglobulin. It belongs to the antibody (Ig) gene family. CD4 is a surface receptor for human immunodeficiency virus (HIV). The CD4 immunoadhesin molecular fusion allow the protein to possess key functions from each independent subunit. The CD4 specific properties include the gp120-binding and HIV-blocking capabilities. Properties specific to immunoglobulin are the long plasma half-life and Fc receptor binding. The properties of the protein means that it has potential to be used in AIDS therapy as of 2017. Specifically, CD4 immunoadhesin plays a role in antibody-dependent cell-mediated cytotoxicity (ADCC) towards HIV-infected cells. While natural anti-gp120 antibodies exhibit a response towards uninfected CD4-expressing cells that have a soluble gp120 bound to the CD4 on the cell surface, CD4 immunoadhesin, however, will not exhibit a response. One of the most relevant of these possibilities is its ability to cross the placenta.
Long-term nonprogressors (LTNPs), are individuals infected with HIV, who maintain a CD4 count greater than 500 without antiretroviral therapy with a detectable viral load. Many of these patients have been HIV positive for 30 years without progressing to the point of needing to take medication in order not to develop AIDS. They have been the subject of a great deal of research, since an understanding of their ability to control HIV infection may lead to the development of immune therapies or a therapeutic vaccine. The classification "Long-term non-progressor" is not permanent, because some patients in this category have gone on to develop AIDS.
AntiViral-HyperActivation Limiting Therapeutics (AV-HALTs) are an investigational class of antiretroviral drugs used to treat Human Immunodeficiency Virus (HIV) infection. Unlike other antiretroviral agents given to reduce viral replication, AV-HALTs are single or combination drugs designed to reduce the rate of viral replication while, at the same time, also directly reducing the state of immune system hyperactivation now believed to drive the loss of CD4+ T helper cells leading to disease progression and Acquired Immunodeficiency Syndrome (AIDS).
HIV/AIDS research includes all medical research that attempts to prevent, treat, or cure HIV/AIDS, as well as fundamental research about the nature of HIV as an infectious agent and AIDS as the disease caused by HIV.
A small proportion of humans show partial or apparently complete innate resistance to HIV, the virus that causes AIDS. The main mechanism is a mutation of the gene encoding CCR5, which acts as a co-receptor for HIV. It is estimated that the proportion of people with some form of resistance to HIV is under 10%.
Gene Martin Shearer is an American immunologist who works at the National Institutes of Health (NIH). He first achieved fame for his discovery in 1974 that T lymphocytes recognized chemically modified surface antigens only in the context of self major histocompatibility complex (MHC) encoded molecules, identifying the central feature of antigen recognition by T lymphocytes known as MHC restriction. His discovery of MHC restriction using chemically modified surface antigens was simultaneous with the discovery of MHC restricted T lymphocyte recognition of virus infected cells by Rolf Zinkernagel and Peter Doherty, who received the 1996 Nobel Prize in Physiology or Medicine.
M. Juliana “Julie” McElrath is a senior vice president and director of the vaccine and infection disease division at Fred Hutchinson Cancer Research Center and the principal investigator of the HIV Vaccine Trials Network Laboratory Center in Seattle, Washington. She is also a professor at the University of Washington.
References
- 1 2 Morgan, D.; C. Mahe; B. Mayanja; J.M. Okongo; R. Lubega; J.A. Whitworth (2002). "HIV-1 infection in rural Africa: is there a difference in median time to AIDS and survival compared with that in industrialized countries?". AIDS. 16 (4): 597–603. doi: 10.1097/00002030-200203080-00011 . PMID 11873003. S2CID 35450422.
- 1 2 Morgan, D.; C. Mahe; B. Mayanja; J.A. Whitworth (2002). "Progression to symptomatic disease in people infected with HIV-1 in rural Uganda: prospective cohort study". BMJ. 324 (7331): 193–196. doi:10.1136/bmj.324.7331.193. ISSN 1180-9639. PMC 64788 . PMID 11809639.
- 1 2 Campbell, G.R.; et al. (2004). "The glutamine-rich region of HIV-1 Tat protein involved in T cell apoptosis". Journal of Biological Chemistry. 279 (46): 48197–48204. doi: 10.1074/jbc.M406195200 . PMID 15331610.
- 1 2 Anzala, O.A.; N.J. Nagelkerke; J.J. Bwayo; D. Holton; S. Moses; E.N. Ngugi; J.O. Ndinya-Achola; F.A. Plummer (1995). "Rapid progression to disease in African sex workers with human immunodeficiency virus type 1 infection". Journal of Infectious Diseases. 171 (3): 686–689. doi:10.1093/infdis/171.3.686. PMID 7876618.
- ↑ N'Galy B, Ryder RW, Bila K, Mwandagalirwa K, Colebunders RL, Francis H, Mann JM, Quinn TC (1988). "Human immunodeficiency virus infection among employees in an African hospital". N. Engl. J. Med. 319 (17): 1123–7. doi:10.1056/NEJM198810273191704. PMID 3262826.
- ↑ Whittle, H.; A. Egboga; J. Todd; T. Corrah; A. Wilkins; E. Demba; G. Morgan; M. Rolfe; N. Berry; R. Tedder (1992). "Clinical and laboratory predictors of survival in Gambian patients with symptomatic HIV-1 or HIV-1 infection". AIDS. 6 (7): 685–689. doi:10.1097/00002030-199207000-00011. PMID 1354448. S2CID 21272316.
- ↑ Marlink, R.; et al. (1994). "Reduced rate of disease development after HIV-2 infection as compared to HIV-1". Science. 265 (5178): 1587–1590. Bibcode:1994Sci...265.1587M. doi:10.1126/science.7915856. PMID 7915856.
- ↑ French, N.; A. Mujugira; J. Nakiyingi; D. Mulder; E.N. Janoff; C.R. Gilks (1999). "Immunologic and clinical stages in HIV-1-infected Ugandan adults are comparable and provide no evidence of rapid progression but poor survival with advanced disease". Journal of Acquired Immune Deficiency Syndromes. 22 (5): 509–516. doi: 10.1097/00126334-199912150-00013 . PMID 10961614.
- ↑ Buchbinder, S.P.; M.H. Katz; N.A. Hessol; P.M. O'Malley; S.D. Holmberg (1994). "Long-term HIV-1 infection without immunologic progression". AIDS. 8 (8): 1123–1128. doi:10.1097/00002030-199408000-00014. PMID 7986410. S2CID 22313180.
- ↑ Cao, Y.; L. Qin; L. Zhang; J. Safrit; D.D. Ho (1995). "Virologic and immunologic characterization of long-term survivors of human immunodeficiency virus type 1 infection". New England Journal of Medicine. 332 (4): 201–208. doi: 10.1056/NEJM199501263320401 . PMID 7808485.
- ↑ Easterbrook, P.J. (1994). "Non-progression in HIV infection". AIDS. 8 (8): 1179–1182. doi:10.1097/00002030-199408000-00023. PMID 7832923.
- ↑ Lévy, J.A. (1993). "HIV pathogenesis and long-term survival". AIDS. 7 (11): 1401–1410. doi:10.1097/00002030-199311000-00001. PMID 8280406.
- 1 2 Harrer, T.; et al. (1996). "Strong cytotoxic T cell and weak neutralizing antibody responses in a subset of persons with stable nonprogressing HIV type 1 infection". AIDS Research and Human Retroviruses. 12 (7): 585–592. doi:10.1089/aid.1996.12.585. PMID 8743084.
- ↑ Deacon, N.J.; et al. (1995). "Genomic structure of an attenuated quasi species of HIV-1 from a blood transfusion donor and recipients". Science. 270 (5238): 988–991. Bibcode:1995Sci...270..988D. doi:10.1126/science.270.5238.988. PMID 7481804. S2CID 37165030.
- ↑ Kirchhoff, F.; T.C. Greenough; D.B. Brettler; J.L. Sullivan; R.C. Desrosiers (1995). "Brief report: absence of intact nef sequences in a long-term survivor with nonprogressive HIV-1 infection". New England Journal of Medicine. 332 (4): 228–232. doi: 10.1056/NEJM199501263320405 . PMID 7808489.
- ↑ Clerici, M.; J.M. Levin; H.A. Kessler; A. Harris; J.A. Berzofsky; A.L. Landay; G.M. Shearer (1994). "HIV-specific T- helper activity in seronegative health care workers exposed to contaminated blood". JAMA. 271 (1): 42–46. doi:10.1001/jama.271.1.42. PMID 8258885.
- ↑ Pinto, L.A.; J. Sullivan; J.A. Berzofsky; M. Clerici; H.A. Kessler; A.L. Landay; G.M. Shearer (1995). "ENV-specific cytotoxic T lymphocyte responses in HIV seronegative health care workers occupationally exposed to HIV-contaminated body fluids". Journal of Clinical Investigation. 96 (2): 867–876. doi:10.1172/JCI118133. PMC 185273 . PMID 7635981.
- ↑ Rowland-Jones, S.; et al. (1995). "HIV-specific cytotoxic T-cells in HIV-exposed but uninfected Gambian women". Nature Medicine. 1 (1): 59–64. doi: 10.1038/nm0195-59 . PMID 7584954. S2CID 10365931.
- ↑ Fowke, K.R.; et al. (1996). "Resistance to HIV-1 infection among persistently seronegative prostitutes in Nairobi, Kenya". Lancet. 348 (9038): 1347–1351. doi:10.1016/S0140-6736(95)12269-2. PMID 8918278. S2CID 21584303.
- ↑ Kaul, R.; et al. (2001). "New insights into HIV-1 specific cytotoxic T cell responses in exposed, persistently seronegative Kenyan sex workers". Immunology Letters. 79 (1–2): 3–13. doi:10.1016/S0165-2478(01)00260-7. PMID 11595284.
- ↑ Koup, R.A.; J.T. Safrit; Y.Z. Cao (1994). "Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome". Journal of Virology. 68 (7): 4650–4655. doi:10.1128/JVI.68.7.4650-4655.1994. PMC 236393 . PMID 8207839.
- ↑ Borrow, P.; H. Lewicki; B.H. Hahn; G.M. Shaw; M.B. Oldstone (1994). "Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection". Journal of Virology. 68 (9): 6103–6110. doi:10.1128/JVI.68.9.6103-6110.1994. PMC 237022 . PMID 8057491.
- ↑ Phillips, R.E.; et al. (1991). "Human immunodeficiency virus genetic variation that can escape cytotoxic T cell recognition". Nature. 354 (6353): 453–459. Bibcode:1991Natur.354..453P. doi: 10.1038/354453a0 . PMID 1721107. S2CID 4257933.
- ↑ Borrow, P.; et al. (1997). "Antiviral pressure exerted by HIV-1-specific cytotoxic T cells (CTLs) during primary infection demonstrated by rapid selection of CTL escape virus". Nature Medicine. 3 (2): 205–211. doi:10.1038/nm0297-205. PMID 9018240. S2CID 8808145.
- ↑ Price, D.A.; P.J. Goulder; P. Klenerman; A.K. Sewell; P.J. Easterbrook; M. Troop; C.R. Bangham; R.E. Phillips (1997). "Positive selection of HIV-1 cytotoxic T lymphocyte escape variants during primary infection". PNAS. 94 (5): 1890–1895. Bibcode:1997PNAS...94.1890P. doi: 10.1073/pnas.94.5.1890 . PMC 20013 . PMID 9050875.
- ↑ Rowland-Jones, S.L.; et al. (1992). "Human immunodeficiency virus variants that escape cytotoxic T-cell recognition". AIDS Research and Human Retroviruses. 8 (9): 1353–1354. doi:10.1089/aid.1992.8.1353. PMID 1466955.
- ↑ Pantaleo, G.; et al. (1997). "The qualitative nature of the primary immune response to HIV infection is a prognosticator of disease progression independent of the initial level of plasma viremia". PNAS. 94 (1): 254–258. Bibcode:1997PNAS...94..254P. doi: 10.1073/pnas.94.1.254 . PMC 19306 . PMID 8990195.
- ↑ Rosenberg, E.S.; J.M. Billingsley; A.M. Caliendo; S.L. Boswell; P.E. Sax; S.A. Kalams; B.D. Walker (1997). "Vigorous HIV-1-specific CD4+ T cell responses associated with control of viremia". Science. 278 (5342): 1447–1450. Bibcode:1997Sci...278.1447R. doi:10.1126/science.278.5342.1447. PMID 9367954.
- ↑ Rowland-Jones, S.L.; et al. (1999). "Broadly cross-reactive HIV-specific cytotoxic T-lymphocytes in highly exposed persistently seronegative donors". Immunology Letters. 66 (1–3): 9–14. doi:10.1016/S0165-2478(98)00179-5. PMID 10203028.
- ↑ Dyer, W.B.; et al. (199). "Strong Human Immunodeficiency Virus (HIV)-Specific Cytotoxic T-Lymphocyte Activity in Sydney Blood Bank Cohort Patients Infected with nef-Defective HIV Type 1". Journal of Virology. 73 (1): 436–443. doi:10.1128/JVI.73.1.436-443.1999. PMC 103850 . PMID 9847349.
- ↑ Kanki, P.J.; et al. (1999). "Human immunodeficiency virus type 1 subtypes differ in disease progression". Journal of Infectious Diseases. 179 (1): 68–73. doi: 10.1086/314557 . PMID 9841824.
- ↑ Kaleebu, P.; et al. (2000). "Molecular epidemiology of HIV type 1 in a rural community in southwest Uganda". AIDS Research and Human Retroviruses. 16 (5): 393–401. doi:10.1089/088922200309052. PMID 10772525.
- ↑ Kaleebu, P.; et al. (2002). "Effect of human immunodeficiency virus (HIV) type 1 envelope subtypes A and D on disease progression in a large cohort of HIV-1-positive persons in Uganda". Journal of Infectious Diseases. 185 (9): 1244–1250. doi: 10.1086/340130 . PMID 12001041.
- ↑ Koblin, B.A.; et al. (1999). "Long-term survival after infection with human immunodeficiency virus type 1 (HIV-1) among homosexual men in hepatitis B vaccine trial cohorts in Amsterdam, New York City, and San Francisco, 1978-1995". American Journal of Epidemiology. 150 (10): 1026–1030. doi: 10.1093/oxfordjournals.aje.a009926 . PMID 10568617.
- ↑ Pezzotti, P.; N. Galai; D. Vlahov; G. Rezza; C.M. Lyles; J. Astemborski (1999). "Direct comparison of time to AIDS and infectious disease death between HIV seroconverter injection drug users in Italy and the United States: results from the ALIVE and ISS studies. AIDS Link to Intravenous Experiences. Italian Seroconversion Study". Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 20 (3): 275–282. doi: 10.1097/00042560-199903010-00010 . PMID 10077177.
- ↑ Collaborative Group on AIDS Incubation and HIV Survival including the CASCADE EU Concerted Action. Concerted Action on SeroConversion to AIDS and Death in Europe (2000). "Time from HIV-1 seroconversion to AIDS and death before widespread use of highly active antiretroviral therapy: a collaborative re-analysis". Lancet. 355 (9210): 1131–1137. doi:10.1016/S0140-6736(00)02061-4. PMID 10791375. S2CID 30898766.
- 1 2 Morgan, D.; G.H. Maude; S.S. Malamba; M.J. Okongo; H.U. Wagner; D.W. Mulder; J.A. Whitworth (1997). "HIV-1 disease progression and AIDS-defining disorders in rural Uganda". Lancet. 350 (9073): 245–250. doi:10.1016/S0140-6736(97)01474-8. PMID 9242801. S2CID 22453416.
- ↑ Gonzalez, E.; et al. (2005). "The influence of CCL3L1 gene-containing segmental duplications on HIV-1/AIDS susceptibility". Science. 307 (5714): 1422–1424. Bibcode:2005Sci...307.1434G. doi:10.1126/science.1101160. PMID 15637236. S2CID 8815153.
- ↑ Lawn, S.D.; S.T. Butera; T.M. Folks (2001). "Contribution of Immune Activation to the Pathogenesis and Transmission of Human Immunodeficiency Virus Type 1 Infection". Clinical Microbiology Reviews. 14 (4): 753–777. doi:10.1128/CMR.14.4.753-777.2001. PMC 89002 . PMID 11585784.
- ↑ Wahl, S.M.; T. Greenwell-Wild; G. Peng; H. Hale-Donze; T.M. Doherty; D. Mizel; J.M. Orenstein (1998). "Mycobacterium avium complex augments macrophage HIV-1 production and increases CCR5 expression". PNAS. 95 (21): 12574–12579. Bibcode:1998PNAS...9512574W. doi: 10.1073/pnas.95.21.12574 . PMC 22872 . PMID 9770527.
- ↑ Juffermans NP, Speelman P, Verbon A, Veenstra J, Jie C, van Deventer SJ, van Der Poll T (2001). "Patients with active tuberculosis have increased expression of HIV coreceptors CXCR4 and CCR5 on CD4(+) T cells" (PDF). Clinical Infectious Diseases. 32 (4): 650–652. doi: 10.1086/318701 . PMID 11181132.
- ↑ Zack, J.A.; S.J. Arrigo; S.R. Weitsman; A.S. Go; A. Haislip; I.S. Chen (1990). "HIV-1 entry into quiescent primary lymphocytes: molecular analysis reveals a labile, latent viral structure". Cell. 61 (2): 213–222. doi:10.1016/0092-8674(90)90802-L. PMID 2331748. S2CID 324887.
- ↑ Kinoshita, S.; B.K. Chen; H. Kaneshima; G.P. Nolan (1998). "Host control of HIV-1 parasitism in T cells by the nuclear factor of activated T cells". Cell. 95 (5): 595–604. doi: 10.1016/S0092-8674(00)81630-X . PMID 9845362. S2CID 17954556.
- ↑ Gaynor, R. (1992). "Cellular transcription factors involved in the regulation of HIV-1 gene expression". AIDS. 6 (4): 347–363. doi:10.1097/00002030-199204000-00001. PMID 1616633.
- ↑ Baeuerle, P.A. (1991). "The inducible transcription activator NF-kappa B: regulation by distinct protein subunits". Biochimica et Biophysica Acta (BBA) - Reviews on Cancer. 1072 (1): 63–80. doi:10.1016/0304-419x(91)90007-8. PMID 2018779.
- ↑ Blanchard, A.; L. Montagnier; M.L. Gougeon (1997). "Influence of microbial infections on the progression of HIV disease". Trends in Microbiology. 5 (8): 326–331. doi:10.1016/S0966-842X(97)01089-5. PMID 9263412.
- ↑ Gendelman, H.E.; et al. (1986). "Trans-activation of the human immunodeficiency virus long terminal repeat sequence by DNA viruses". PNAS. 83 (24): 9759–9763. Bibcode:1986PNAS...83.9759G. doi: 10.1073/pnas.83.24.9759 . PMC 387220 . PMID 2432602.
- ↑ Bentwich, Z.; A. Kalinkovich; Z. Weisman (1995). "Immune activation is a dominant factor in the pathogenesis of African AIDS". Immunology Today. 16 (4): 187–191. doi:10.1016/0167-5699(95)80119-7. PMID 7734046.
- ↑ Maggi, E.; et al. (1994). "Ability of HIV to promote a TH1 to TH0 shift and to replicate preferentially in TH2 and TH0 cells". Science. 265 (5169): 244–248. doi:10.1126/science.8023142. PMID 8023142.