The pericardium, also called pericardial sac, is a double-walled sac containing the heart and the roots of the great vessels. It has two layers, an outer layer made of strong inelastic connective tissue, and an inner layer made of serous membrane. It encloses the pericardial cavity, which contains pericardial fluid, and defines the middle mediastinum. It separates the heart from interference of other structures, protects it against infection and blunt trauma, and lubricates the heart's movements.
The azygos vein is a vein running up the right side of the thoracic vertebral column draining itself towards the superior vena cava. It connects the systems of superior vena cava and inferior vena cava and can provide an alternative path for blood to the right atrium when either of the venae cavae is blocked.
The Pemberton's sign is a physical examination tool used to demonstrate the presence of latent pressure in the thoracic inlet. The sign is named after Hugh Pemberton, who characterized it in 1946.
Radiology (X-rays) is used in the diagnosis of tuberculosis. Abnormalities on chest radiographs may be suggestive of, but are never diagnostic of TB, but can be used to rule out pulmonary TB.

A thoracotomy is a surgical procedure to gain access into the pleural space of the chest. It is performed by surgeons to gain access to the thoracic organs, most commonly the heart, the lungs, or the esophagus, or for access to the thoracic aorta or the anterior spine. A thoracotomy is the first step in thoracic surgeries including lobectomy or pneumonectomy for lung cancer or to gain thoracic access in major trauma.

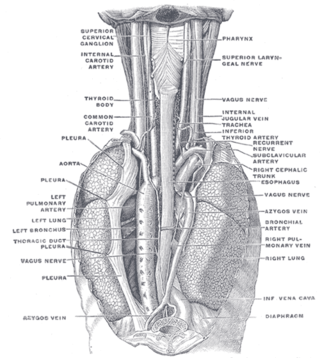
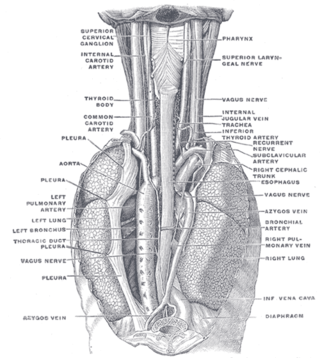
The mediastinum is the central compartment of the thoracic cavity. Surrounded by loose connective tissue, it is a region that contains vital organs and structures within the thorax, namely the heart and its vessels, the esophagus, the trachea, the vagus, phrenic and cardiac nerves, the thoracic duct, the thymus and the lymph nodes of the central chest.

A chest radiograph, chest X-ray (CXR), or chest film is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

Esophageal rupture, also known as Boerhaave syndrome, is a rupture of the esophageal wall. Iatrogenic causes account for approximately 56% of esophageal perforations, usually due to medical instrumentation such as an endoscopy or paraesophageal surgery. The 10% of esophageal perforations caused specifically by vomiting are termed Boerhaave syndrome.

A pancreatic fistula is an abnormal communication between the pancreas and other organs due to leakage of pancreatic secretions from damaged pancreatic ducts. An external pancreatic fistula is one that communicates with the skin, and is also known as a pancreaticocutaneous fistula, whereas an internal pancreatic fistula communicates with other internal organs or spaces. Pancreatic fistulas can be caused by pancreatic disease, trauma, or surgery.

Mediastinitis is inflammation of the tissues in the mid-chest, or mediastinum. It can be either acute or chronic. It is thought to be due to four different etiologies:

Pneumomediastinum is pneumatosis in the mediastinum, the central part of the chest cavity. First described in 1819 by René Laennec, the condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity. In underwater divers it is usually the result of pulmonary barotrauma.

A mediastinal tumor is a tumor in the mediastinum, the cavity that separates the lungs from the rest of the chest. It contains the heart, esophagus, trachea, thymus, and aorta. The most common mediastinal masses are thymoma, usually found in the anterior mediastinum, followed by neurogenic Timor (15–20%) located in the anterior mediastinum. Lung cancer typically spreads to the lymph nodes in the mediastinum.
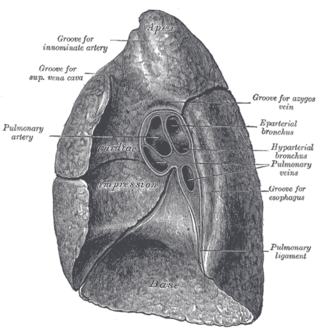
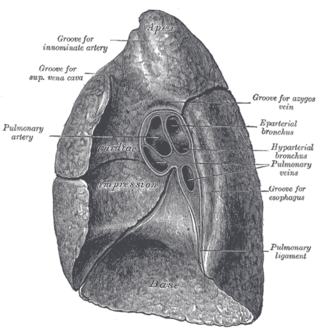
The root of the lung is a group of structures that emerge at the hilum of each lung, just above the middle of the mediastinal surface and behind the cardiac impression of the lung. It is nearer to the back than the front. The root of the lung is connected by the structures that form it to the heart and the trachea. The rib cage is separated from the lung by a two-layered membranous coating, the pleura. The hilum is the large triangular depression where the connection between the parietal pleura and the visceral pleura is made, and this marks the meeting point between the mediastinum and the pleural cavities.
Mediastinal germ cell tumors are tumors that derive from germ cell rest remnants in the mediastinum. Germ cell tumors most commonly occur in the gonad but occasionally elsewhere.

Pneumopericardium is a medical condition where air enters the pericardial cavity. This condition has been recognized in preterm neonates, in which it is associated with severe lung pathology, after vigorous resuscitation, or in the presence of assisted ventilation. This is a serious complication, which if untreated may lead to cardiac tamponade and death. Pneumomediastinum, which is the presence of air in the mediastinum, may mimic and also coexist with pneumopericardium.
Lung cancer staging is the assessment of the extent to which a lung cancer has spread from its original source. As with most cancers, staging is an important determinant of treatment and prognosis. In general, more advanced stages of cancer are less amenable to treatment and have a worse prognosis.

Subcutaneous emphysema occurs when gas or air accumulates and seeps under the skin, where normally no gas should be present. Subcutaneous refers to the subcutaneous tissue, and emphysema refers to trapped air pockets. Since the air generally comes from the chest cavity, subcutaneous emphysema usually occurs around the upper torso, such as on the chest, neck, face, axillae and arms, where it is able to travel with little resistance along the loose connective tissue within the superficial fascia. Subcutaneous emphysema has a characteristic crackling-feel to the touch, a sensation that has been described as similar to touching warm Rice Krispies. This sensation of air under the skin is known as subcutaneous crepitation, a form of crepitus.

The pleurae are the two flattened closed sacs filled with pleural fluid, each ensheathing each lung and lining their surrounding tissues, locally appearing as two opposing layers of serous membrane separating the lungs from the mediastinum, the inside surfaces of the surrounding chest walls and the diaphragm. Although wrapped onto itself resulting in an apparent double layer, each lung is surrounded by a single, continuous pleural membrane.

Mediastinal shift is an abnormal movement of the mediastinal structures toward one side of the chest cavity. A shift indicates a severe imbalance of pressures inside the chest. Mediastinal shifts are generally caused by increased lung volume, decreased lung volume, or abnormalities in the pleural space. Additionally, masses inside the mediastinum or musculoskeletal abnormalities can also lead to abnormal mediastinal arrangement. Typically, these shifts are observed on x-ray but also on computed tomography (CT) or magnetic resonance imaging (MRI). On chest x-ray, tracheal deviation, or movement of the trachea away from its midline position can be used as a sign of a shift. Other structures, like the heart, can also be used as reference points. Below are examples of pathologies that can cause a mediastinal shift and their appearance.

The aortopulmonary space is a small space between the aortic arch and the pulmonary artery. It contains the ligamentum arteriosum, the recurrent laryngeal nerve, lymph nodes, and fatty tissue. The space is bounded anteriorly by the ascending aorta, posteriorly by the descending aorta, medially by the left main bronchus, and laterally by mediastinal pleura.