
An antacid is a substance which neutralizes stomach acidity and is used to relieve heartburn, indigestion or an upset stomach. Some antacids have been used in the treatment of constipation and diarrhea. Marketed antacids contain salts of aluminum, calcium, magnesium, or sodium. Some preparations contain a combination of two salts, such as magnesium carbonate and aluminium hydroxide.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.
Heller myotomy is a surgical procedure in which the muscles of the cardia are cut, allowing food and liquids to pass to the stomach. It is used to treat achalasia, a disorder in which the lower esophageal sphincter fails to relax properly, making it difficult for food and liquids to reach the stomach.

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is one of the upper gastrointestinal chronic diseases in which stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. In the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.

Barrett's esophagus is a condition in which there is an abnormal (metaplastic) change in the mucosal cells lining the lower portion of the esophagus, from stratified squamous epithelium to simple columnar epithelium with interspersed goblet cells that are normally present only in the small intestine and large intestine. This change is considered to be a premalignant condition because it is associated with a high incidence of further transition to esophageal adenocarcinoma, an often-deadly cancer.
A hiatal hernia or hiatus hernia is a type of hernia in which abdominal organs slip through the diaphragm into the middle compartment of the chest. This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn. Other symptoms may include trouble swallowing and chest pains. Complications may include iron deficiency anemia, volvulus, or bowel obstruction.
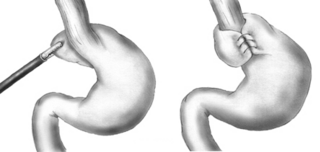
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.

Robot-assisted surgery or robotic surgery are any types of surgical procedures that are performed using robotic systems. Robotically assisted surgery was developed to try to overcome the limitations of pre-existing minimally-invasive surgical procedures and to enhance the capabilities of surgeons performing open surgery.
Stretta is a minimally invasive endoscopic procedure for the treatment of gastroesophageal reflux disease (GERD) that delivers radiofrequency energy in the form of electromagnetic waves through electrodes at the end of a catheter to the lower esophageal sphincter (LES) and the gastric cardia – the region of the stomach just below the LES. The energy heats the tissue, ultimately causing it to swell and stiffen; the way this works was not understood as of 2015, but it was thought that perhaps the heat causes local inflammation, collagen deposition and muscular thickening of the LES and that it may disrupt the nerves there.
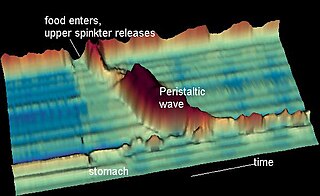
Nutcracker esophagus, jackhammer esophagus, or hypercontractile peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, with both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.
Sandifer syndrome is an eponymous paediatric medical disorder, characterised by gastrointestinal symptoms and associated neurological features. There is a significant correlation between the syndrome and gastro-oesophageal reflux disease (GORD); however, it is estimated to occur in less than 1% of children with reflux.
Norman Rupert Barrett CBE FRSA was an Australian-born British thoracic surgeon who is widely yet mistakenly remembered for describing what became known as Barrett's oesophagus.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
A Collis gastroplasty is a surgical procedure performed when the surgeon desires to create a Nissen fundoplication, but the portion of esophagus inferior to the diaphragm is too short. Thus, there is not enough esophagus to wrap. A vertical incision is made in the stomach parallel to the left border of the esophagus. This effectively lengthens the esophagus. The stomach fundus can then be wrapped around the neo-esophagus, thus reducing reflux of stomach acid into the esophagus.

Rudolph Nissen was a German surgeon who chaired surgery departments in Turkey, the United States and Switzerland. The Nissen fundoplication, a surgical procedure for the treatment of gastroesophageal reflux disease, is named after him.
Stomach Intestinal Pylorus-Sparing (SIPS) surgery is a type of weight-loss surgery. It was developed in 2013 by two U.S. surgeons, Daniel Cottam from Utah and Mitchell S. Roslin from New York.
The per-oral endoscopic myotomy, or POEM, is a minimally invasive surgical procedure for the treatment of achalasia wherein the inner circular muscle layer of the lower esophageal sphincter is divided through a submucosal tunnel. This enables food and liquids to pass into the stomach, a process that is impaired in achalasia. The tunnel is created, and the myotomy performed, using a flexible endoscope, meaning the entire procedure can be done without external incisions.
Transoral incisionless fundoplication (TIF) is an endoscope treatment designed to relieve symptoms of gastroesophageal reflux disease (GERD). The TIF procedure, similar to Nissen fundoplication, alleviates GERD symptoms by wrapping a portion of the stomach around the esophagus.

Morio Kasai was a Japanese surgeon who had a strong interest in pediatric surgery. While Kasai went into practice at a time when pediatric surgery was not an established subspecialty, much of his clinical and research work was related to the surgical care of children. He is best known for devising a surgical procedure, the hepatoportoenterostomy, to address a life-threatening birth defect known as biliary atresia. The modern form of the operation is still known as the Kasai procedure.

Haruhiro Inoue is a Japanese thoracic surgeon and endoscopist best known for the development of the cap endoscopic mucosal resection technique, and the first per-oral endoscopic myotomy performed in humans. He is a professor at Showa University and Director of the Digestive Disease Centre at Showa University Koto-Toyosu Hospital in Tokyo. He is known for his work in endoscopy and his contribution to the development of endoscopic technologies and procedures.