Related Research Articles

Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in a brachial artery, where it is most commonly measured. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure, or in kilopascals (kPa). The difference between the systolic and diastolic pressures is known as pulse pressure, while the average pressure during a cardiac cycle is known as mean arterial pressure.
Orthostatic hypotension, also known as postural hypotension, is a medical condition wherein a person's blood pressure drops when standing up or sitting down. Primary orthostatic hypotension is also often referred to as neurogenic orthostatic hypotension. The drop in blood pressure may be sudden, within 3 minutes or gradual. It is defined as a fall in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. It occurs predominantly by delayed constriction of the lower body blood vessels, which is normally required to maintain adequate blood pressure when changing the position to standing. As a result, blood pools in the blood vessels of the legs for a longer period, and less is returned to the heart, thereby leading to a reduced cardiac output and inadequate blood flow to the brain.

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.
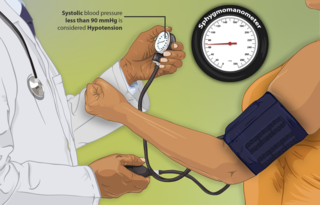
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures within the cardiac cycle, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.

Postural orthostatic tachycardia syndrome (POTS) is a condition characterized by an abnormally large increase in heart rate upon sitting up or standing. POTS is a disorder of the autonomic nervous system that can lead the individual to experience a variety of symptoms. Symptoms may include lightheadedness, brain fog, blurred vision, weakness, fatigue, headaches, heart palpitations, exercise intolerance, nausea, diminished concentration, tremulousness (shaking), syncope (fainting), coldness or pain in the extremities, chest pain and shortness of breath. Other conditions associated with POTS include migraine headaches, Ehlers–Danlos syndrome, asthma, autoimmune disease, vasovagal syncope and mast cell activation syndrome. POTS symptoms may be treated with lifestyle changes such as increasing fluid and salt intake, wearing compression stockings, gentler and slow postural changes, avoiding prolonged bedrest, medication and physical therapy.

Neurogenic shock is a distributive type of shock resulting in hypotension, often with bradycardia, caused by disruption of autonomic nervous system pathways. It can occur after damage to the central nervous system, such as spinal cord injury and traumatic brain injury. Low blood pressure occurs due to decreased systemic vascular resistance resulting from loss of sympathetic tone, which in turn causes blood pooling within the extremities rather than being available to circulate throughout the body. The slowed heart rate results from a vagal response unopposed by a sympathetic nervous system (SNS) response. Such cardiovascular instability is exacerbated by hypoxia, or treatment with endotracheal or endobronchial suction used to prevent pulmonary aspiration.

Vital signs are a group of the four to six most crucial medical signs that indicate the status of the body's vital (life-sustaining) functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person's vital signs vary with age, weight, sex, and overall health.

Midodrine is a vasopressor/antihypotensive agent. Midodrine was approved in the United States by the Food and Drug Administration (FDA) in 1996 for the treatment of dysautonomia and orthostatic hypotension. In August 2010, the FDA proposed withdrawing this approval because the manufacturer, Shire plc, failed to complete required studies after the medicine reached the market. In September 2010, the FDA reversed its decision to remove midodrine from the market and allowed it to remain available to patients while Shire plc collected further data regarding the efficacy and safety of the drug. Shire announced on September 22, 2011, that it was withdrawing completely from supplying midodrine and leaving it to several generics to supply the drug.

A tilt table test (TTT), occasionally called upright tilt testing (UTT), is a medical procedure often used to diagnose dysautonomia or syncope. Patients with symptoms of dizziness or lightheadedness, with or without a loss of consciousness (fainting), suspected to be associated with a drop in blood pressure or positional tachycardia are good candidates for this test.

Pure autonomic failure (PAF) is an uncommon, sporadic neurodegenerative condition marked by a steadily declining autonomic regulation. Bradbury and Eggleston originally described pure autonomic failure in 1925.
A post-anesthesia care unit (PACU) and sometimes referred to as post-anesthesia recovery or PAR, or simply recovery, is a part of hospitals, ambulatory care centers, and other medical facilities. Patients who received general anesthesia, regional anesthesia, or local anesthesia are transferred from the operating room suites to the recovery area. The patients are monitored typically by anesthesiologists, nurse anesthetists, and other medical staff. Providers follow a standardized handoff to the medical PACU staff that includes, which medications were given in the operating room suites, how hemodynamics were during the procedures, and what is expected for their recovery. After initial assessment and stabilization, patients are monitored for any potential complications, until the patient is transferred back to their hospital rooms.

Droxidopa is a synthetic amino acid precursor which acts as a prodrug to the neurotransmitter norepinephrine (noradrenaline). Unlike norepinephrine, droxidopa is capable of crossing the protective blood–brain barrier (BBB).

Syncope, commonly known as fainting or passing out, is a loss of consciousness and muscle strength characterized by a fast onset, short duration, and spontaneous recovery. It is caused by a decrease in blood flow to the brain, typically from low blood pressure. There are sometimes symptoms before the loss of consciousness such as lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm. Syncope may also be associated with a short episode of muscle twitching. Psychiatric causes can also be determined when a patient experiences fear, anxiety, or panic; particularly before a stressful event, usually medical in nature. When consciousness and muscle strength are not completely lost, it is called presyncope. It is recommended that presyncope be treated the same as syncope.
Orthostatic syncope refers to syncope resulting from a postural decrease in blood pressure, termed orthostatic hypotension.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50 mmHg or systolic blood pressure of less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury, some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding are thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.
Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.

Arterial blood pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure. Blood pressure values are generally reported in millimetres of mercury (mmHg), though aneroid and electronic devices do not contain mercury.
Supine hypertension is a paradoxical elevation in blood pressure upon assuming a supine position from a standing or sitting position. It is assumed to be a manifestation of disorders of the autonomic nervous system or due to side effects of medications such as midodrine and droxidopa.
References
- ↑ https://www.cdc.gov/steadi/pdf/STEADI-Assessment-MeasuringBP-508.pdf [ bare URL PDF ]
- 1 2 3 Grossman, Valerie G. A. (1 April 2003). Quick reference to triage. Lippincott Williams & Wilkins. p. 12. ISBN 978-0-7817-4022-7 . Retrieved 11 May 2010.
- ↑ Beebe, Richard W. O.; Deborah L. Funk (6 March 2001). Fundamentals of emergency care. Cengage Learning. p. 219. ISBN 978-0-7668-1498-1 . Retrieved 11 May 2010.
- ↑ Knies, Robert C. "Orthostatic Measurement". Emergency Nursing World!. Retrieved 2010-05-11.
- 1 2 Beebe and Funk (2001), 218.
- ↑ Bailey, James. "Hemodynamic instability". Clinical Window. GE Healthcare. Archived from the original on 10 May 2010.
- 1 2 Hubbell, Kelly A.; Andrea Novak; Emergency Nurses Association (25 April 2002). Emergency Care Technician Curriculum. Jones & Bartlett Learning. p. 14. ISBN 978-0-7637-1913-5 . Retrieved 11 May 2010.