In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

Compartment syndrome is a condition in which increased pressure within one of the body's anatomical compartments results in insufficient blood supply to tissue within that space. There are two main types: acute and chronic. Compartments of the leg or arm are most commonly involved.
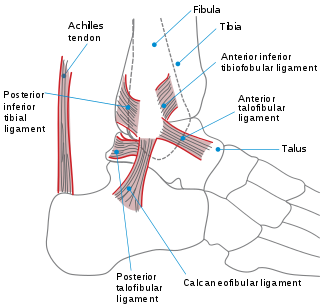
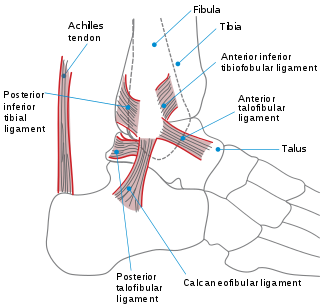
The ankle, or the talocrural region, or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joint. The movements produced at this joint are dorsiflexion and plantarflexion of the foot. In common usage, the term ankle refers exclusively to the ankle region. In medical terminology, "ankle" can refer broadly to the region or specifically to the talocrural joint.

A bone fracture is a medical condition in which there is a partial or complete break in the continuity of any bone in the body. In more severe cases, the bone may be broken into several fragments, known as a comminuted fracture. A bone fracture may be the result of high force impact or stress, or a minimal trauma injury as a result of certain medical conditions that weaken the bones, such as osteoporosis, osteopenia, bone cancer, or osteogenesis imperfecta, where the fracture is then properly termed a pathologic fracture.

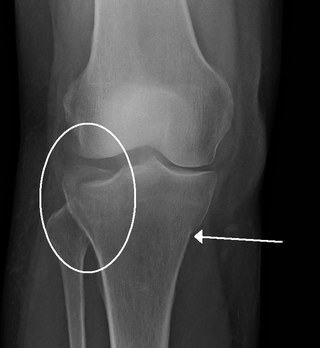
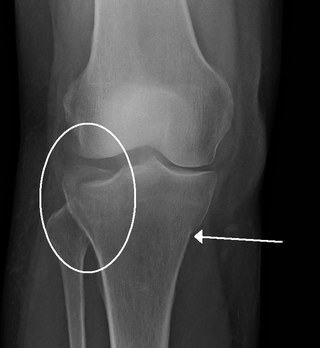
The Maisonneuve fracture is a spiral fracture of the proximal third of the fibula associated with a tear of the distal tibiofibular syndesmosis and the interosseous membrane. There is an associated fracture of the medial malleolus or rupture of the deep deltoid ligament of the ankle. This type of injury can be difficult to detect.

A distal radius fracture, also known as wrist fracture, is a break of the part of the radius bone which is close to the wrist. Symptoms include pain, bruising, and rapid-onset swelling. The ulna bone may also be broken.

A shin splint, also known as medial tibial stress syndrome, is pain along the inside edge of the shinbone (tibia) due to inflammation of tissue in the area. Generally this is between the middle of the lower leg and the ankle. The pain may be dull or sharp, and is generally brought on by high-impact exercise that overloads the tibia. It generally resolves during periods of rest. Complications may include stress fractures.

The tibialis posterior muscle is the most central of all the leg muscles, and is located in the deep posterior compartment of the leg. It is the key stabilizing muscle of the lower leg.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.

Osteochondritis dissecans is a joint disorder primarily of the subchondral bone in which cracks form in the articular cartilage and the underlying subchondral bone. OCD usually causes pain during and after sports. In later stages of the disorder there will be swelling of the affected joint which catches and locks during movement. Physical examination in the early stages does only show pain as symptom, in later stages there could be an effusion, tenderness, and a crackling sound with joint movement.

A patella fracture is a break of the kneecap. Symptoms include pain, swelling, and bruising to the front of the knee. A person may also be unable to walk. Complications may include injury to the tibia, femur, or knee ligaments.

A malleolus is the bony prominence on each side of the human ankle.

A calcaneal fracture is a break of the calcaneus. Symptoms may include pain, bruising, trouble walking, and deformity of the heel. It may be associated with breaks of the hip or back.

A trimalleolar fracture is a fracture of the ankle that involves the lateral malleolus, the medial malleolus, and the distal posterior aspect of the tibia, which can be termed the posterior malleolus. The trauma is sometimes accompanied by ligament damage and dislocation.

An open fracture, also called a compound fracture, is a type of bone fracture that has an open wound in the skin near the fractured bone. The skin wound is usually caused by the bone breaking through the surface of the skin. Open fractures are emergencies and are often caused by high energy trauma such as road traffic accidents and are associated with a high degree of damage to the bone and nearby soft tissue. An open fracture can be life threatening or limb-threatening due to the risk of a deep infection and/or bleeding. Other complications including a risk of malunion of the bone or nonunion of the bone. The severity of open fractures can vary. For diagnosing and classifying open fractures, Gustilo-Anderson open fracture classification is the most commonly used method. It can also be used to guide treatment, and to predict clinical outcomes. Advanced trauma life support is the first line of action in dealing with open fractures and to rule out other life-threatening condition in cases of trauma. The person is also administered antibiotics for at least 24 hours to reduce the risk of an infection. Cephalosporins are generally the first line of antibiotics. Therapeutic irrigation, wound debridement, early wound closure and bone fixation are the main management of open fractures. All these actions aimed to reduce the risk of infections. The bone that is most commonly injured is the tibia and working-age young men are the group of people who are at highest risk of an open fracture. Older people with osteoporosis and soft-tissue problems are also at risk.

Mandibular fracture, also known as fracture of the jaw, is a break through the mandibular bone. In about 60% of cases the break occurs in two places. It may result in a decreased ability to fully open the mouth. Often the teeth will not feel properly aligned or there may be bleeding of the gums. Mandibular fractures occur most commonly among males in their 30s.
The Gustilo open fracture classification system is the most commonly used classification system for open fractures. It was created by Ramón Gustilo and Anderson, and then further expanded by Gustilo, Mendoza, and Williams.
A crus fracture is a fracture of the lower legs bones meaning either or both of the tibia and fibula.

A tibial plateau fracture is a break of the upper part of the tibia (shinbone) that involves the knee joint. Symptoms include pain, swelling, and a decreased ability to move the knee. People are generally unable to walk. Complication may include injury to the artery or nerve, arthritis, and compartment syndrome.

Tibia shaft fracture is a fracture of the proximal (upper) third of the tibia. Due to the location of the tibia, it is frequently injured. Thus it is the most commonly fractured long bone in the body.