Androgen insensitivity syndrome (AIS) is a difference in sex development involving hormonal resistance due to androgen receptor dysfunction.
Virilization or masculinization is the biological development of adult male characteristics in young males or females. Most of the changes of virilization are produced by androgens.

Intersex medical interventions, also known as intersex genital mutilations (IGM), are surgical, hormonal and other medical interventions performed to modify atypical or ambiguous genitalia and other sex characteristics, primarily for the purposes of making a person's appearance more typical and to reduce the likelihood of future problems. The history of intersex surgery has been characterized by controversy due to reports that surgery can compromise sexual function and sensation, and create lifelong health issues. Timing, evidence, necessity and indications for surgeries in infancy, adolescence or adult age have been controversial, associated with issues of consent.

The history of intersex surgery is intertwined with the development of the specialities of pediatric surgery, pediatric urology, and pediatric endocrinology, with our increasingly refined understanding of sexual differentiation, with the development of political advocacy groups united by a human qualified analysis, and in the last decade by doubts as to efficacy, and controversy over when and even whether some procedures should be performed.

Clitoromegaly is an abnormal enlargement of the clitoris that is mostly congenital or acquired, though deliberately induced clitoris enlargement as a form of genital body modification is achieved through various uses of anabolic steroids, including testosterone. Clitoromegaly is not the same as normal enlargement of the clitoris seen during sexual arousal.

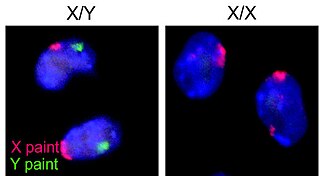
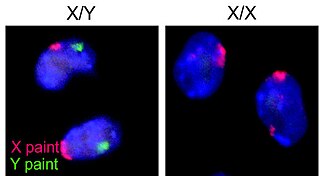
XX male syndrome, also known as de la Chapelle syndrome, is a rare congenital intersex condition in which an individual with a 46,XX karyotype has phenotypically male characteristics that can vary among cases. Synonyms include 46,XX testicular difference of sex development, 46,XX sex reversal, nonsyndromic 46,XX testicular DSD, and XX sex reversal.

Partial androgen insensitivity syndrome (PAIS) is a condition that results in the partial inability of the cell to respond to androgens. It is an X linked recessive condition. The partial unresponsiveness of the cell to the presence of androgenic hormones impairs the masculinization of male genitalia in the developing fetus, as well as the development of male secondary sexual characteristics at puberty, but does not significantly impair female genital or sexual development. As such, the insensitivity to androgens is clinically significant only when it occurs in individuals with a Y chromosome. Clinical features include ambiguous genitalia at birth and primary amenhorrhoea with clitoromegaly with inguinal masses. Mullerian structures are not present in the individual.
Pseudohermaphroditism is a condition in which an individual has a matching chromosomal and gonadal tissue sex, but mismatching external genitalia.

Disorders of sex development (DSDs), also known as differences in sex development, diverse sex development and variations in sex characteristics (VSC), are congenital conditions affecting the reproductive system, in which development of chromosomal, gonadal, or anatomical sex is atypical.

Complete androgen insensitivity syndrome (CAIS) is an AIS condition that results in the complete inability of the cell to respond to androgens. As such, the insensitivity to androgens is only clinically significant when it occurs in individuals who are exposed to significant amounts of testosterone at some point in their lives. The unresponsiveness of the cell to the presence of androgenic hormones prevents the masculinization of male genitalia in the developing fetus, as well as the development of male secondary sexual characteristics at puberty, but does allow, without significant impairment, female genital and sexual development in those with the condition.

Intersex people are individuals born with any of several sex characteristics including chromosome patterns, gonads, or genitals that, according to the Office of the United Nations High Commissioner for Human Rights, "do not fit typical binary notions of male or female bodies".

Mild androgen insensitivity syndrome (MAIS) is a condition that results in a mild impairment of the cell's ability to respond to androgens. The degree of impairment is sufficient to impair spermatogenesis and / or the development of secondary sexual characteristics at puberty in males, but does not affect genital differentiation or development. Female genital and sexual development is not significantly affected by the insensitivity to androgens; as such, MAIS is only diagnosed in males. The clinical phenotype associated with MAIS is a normal male habitus with mild spermatogenic defect and / or reduced secondary terminal hair.

Isolated 17,20-lyase deficiency (ILD), also called isolated 17,20-desmolase deficiency, is a rare endocrine and autosomal recessive genetic disorder which is characterized by a complete or partial loss of 17,20-lyase activity and, in turn, impaired production of the androgen and estrogen sex steroids. The condition manifests itself as pseudohermaphroditism in males, in whom it is considered to be a form of intersex, and, in both sexes, as a reduced or absent puberty/lack of development of secondary sexual characteristics, resulting in a somewhat childlike appearance in adulthood.

The Prader scale or Prader staging, named after Andrea Prader, is a coarse rating system for the measurement of the degree of virilization of the genitalia of the human body and is similar to the Quigley scale. It primarily relates to virilization of the female genitalia in cases of congenital adrenal hyperplasia (CAH) and identifies five distinct stages, but in recent times has been used to describe the range of differentiation of genitalia, with normal infant presentation being shown on either end of the scale, female on the left (0) and male on the right (6).
The Phall-O-meter is a satirical measure that critiques medical standards for normal male and female phalluses. The tool was developed by Kiira Triea based on a concept by Suzanne Kessler and is used to demonstrate concerns with the medical treatment of intersex bodies.
Intersex Peer Support Australia (IPSA), also known as the Androgen Insensitivity Syndrome Support Group Australia, is possibly the oldest known intersex organization, established in 1985. It provides peer and family support, information and advocacy. The group is run by volunteers, for people with intersex variations such as androgen insensitivity syndrome. It changed name from the Androgen Insensitivity Syndrome Support Group Australia (AISSGA) to Intersex Peer Support Australia in 2019.

Intersex people in the United Kingdom face significant gaps in legal protections, particularly in protection from non-consensual medical interventions, and protection from discrimination. Actions by intersex civil society organisations aim to eliminate unnecessary medical interventions and harmful practices, promote social acceptance, and equality in line with Council of Europe and United Nations demands. Intersex civil society organisations campaign for greater social acceptance, understanding of issues of bodily autonomy, and recognition of the human rights of intersex people.

Intersex people are born with natural variations in physical and sex characteristics including those of the chromosomes, gonads, sex hormones, or genitals that, according to the UN Office of the High Commissioner for Human Rights, "do not fit the typical definitions for male or female bodies". Such variations may involve genital ambiguity, and combinations of chromosomal genotype and sexual phenotype other than XY-male and XX-female. Preimplantation genetic diagnosis allows the elimination of embryos and fetuses with intersex traits and thus has an impact on discrimination against intersex people.
Sexual anomalies, also known as sexual abnormalities, are a set of clinical conditions due to chromosomal, gonadal and/or genitalia variation. Individuals with congenital (inborn) discrepancy between sex chromosome, gonadal, and their internal and external genitalia are categorised as individuals with a disorder of sex development (DSD). Afterwards, if the family or individual wishes, they can partake in different management and treatment options for their conditions.

The definition of what is an intersex condition is controversial. Ambiguous genitalia occurs in roughly 0.05% of all births, and atypical genitalia occurs in 0.5% of all births, usually caused by masculinization or feminization during pregnancy, these conditions range from full androgen insensitivity syndrome, to ovotesticular syndrome although the definition of "normal" genitalia is largely arbitrary. 1.7% of people are born with a difference of sexual development, such as those with Klinefelter's syndrome. The DSD was specifically made to be as inclusive to all atypical sexual development, not all conditions within the DSD effect individuals to the same extent. Most intersex activism is based around the end of unnecessary medical interventions on intersex youth which attempt to assign an arbitrary sex and gender binary often causing physical harm with no input from the child. Intersex conditions are usually expanded to include the DSD more generally. While 0.5% of all births are born with atypical genitalia only 0.05% of births are medically treated, or considered to be "truly" ambiguous generally.