| Complete androgen insensitivity syndrome | |
|---|---|
| Other names | Complete androgen resistance syndrome |
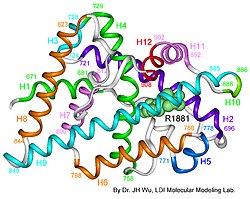 | |
| AIS results when the function of the androgen receptor (AR) is impaired. The AR protein (pictured) mediates the effects of androgens in the human body. | |
| Specialty | Gynaecology, endocrinology |
Complete androgen insensitivity syndrome (CAIS) is an AIS condition that results in the complete inability of the cell to respond to androgens. [1] [2] [3] As such, the insensitivity to androgens is only clinically significant when it occurs in individuals who are exposed to significant amounts of testosterone at some point in their lives. [1] The unresponsiveness of the cell to the presence of androgenic hormones prevents the masculinization of male genitalia in the developing fetus, as well as the development of male secondary sexual characteristics at puberty, but does allow, without significant impairment, female genital and sexual development [3] [4] in those with the condition.
Contents
- Signs and symptoms
- Physical
- Endocrine
- Comorbidity
- Diagnosis
- Management
- Sex assignment and sexuality
- Dilation therapy
- Gonadectomy
- Hormone replacement therapy
- Counseling
- Neovaginal construction
- Prognosis
- Epidemiology
- Nomenclature
- History
- People with CAIS
- See also
- References
- External links
All human fetuses begin fetal development looking similar, with both the Müllerian duct system (female) and the Wolffian duct system (male) developing. Sex differentiation begins with the gonads, which in XX individuals become ovaries, and in XY individuals (including those with CAIS) typically become testicles due to the presence of the Y chromosome. It is at the seventh week of gestation that the bodies of non-CAIS individuals with the XY karyotype begin their masculinization: i.e., the Wolffian duct system is promoted and the Müllerian duct system is suppressed (the reverse happens with typically developing females). This process is triggered by androgens produced by the testicles. The bodies of unaffected XY individuals masculinize by, among other things, enlarging the genital tubercle into a penis, which in females becomes the clitoris, while what in females becomes the labia fuses to become the scrotum of males (where the testicles will later descend). [ citation needed ]
XY individuals affected by CAIS develop a normal external female habitus, despite the presence of a Y chromosome, [1] [5] [6] [7] [8] [9] but internally, they will lack a uterus, and the vaginal cavity will be shallow, while the gonads, which differentiated into testes in the earlier separate process also triggered by their Y chromosome, will remain undescended in the place. This results not only in infertility in individuals with CAIS, but also presents a risk of gonadal cancer later on in life. [10]
CAIS is one of the three categories of androgen insensitivity syndrome (AIS) since AIS is differentiated according to the degree of genital masculinization: complete androgen insensitivity syndrome (CAIS) when the external genitalia is that of a typical female, mild androgen insensitivity syndrome (MAIS) when the external genitalia is that of a typical male, and partial androgen insensitivity syndrome (PAIS) when the external genitalia is partially, but not fully masculinized. [1] [2] [5] [6] [7] [11] [12] [13] [14]
Androgen insensitivity syndrome is the largest single entity that leads to 46, XY undermasculinization. [15]





