Related Research Articles

Cyanosis is the change of body tissue color to a bluish-purple hue as a result of having decreased amounts of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Body tissues that show cyanosis are usually in locations where the skin is thinner, including the mucous membranes, lips, nail beds, and ear lobes. Some medications containing amiodarone or silver, Mongolian spots, large birth marks, and the consumption of food products with blue or purple dyes can also result in the bluish skin tissue discoloration and may be mistaken for cyanosis.

Peripheral artery disease (PAD) is an abnormal narrowing of arteries other than those that supply the heart or brain. PAD can happen in any blood vessel, but it is more common in the legs than the arms.
Intermittent claudication, also known as vascular claudication, is a symptom that describes muscle pain on mild exertion, classically in the calf muscle, which occurs during exercise, such as walking, and is relieved by a short period of rest. It is classically associated with early-stage peripheral artery disease, and can progress to critical limb ischemia unless treated or risk factors are modified and maintained.
Claudication is a medical term usually referring to impairment in walking, or pain, discomfort, numbness, or tiredness in the legs that occurs during walking or standing and is relieved by rest. The perceived level of pain from claudication can be mild to extremely severe. Claudication is most common in the calves but it can also affect the feet, thighs, hips, buttocks, or arms. The word claudication comes from the Latin claudicare meaning 'to limp'.
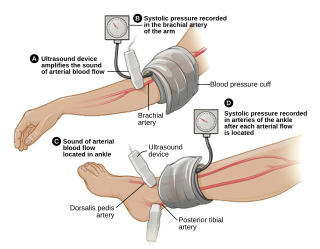
The ankle-brachial pressure index (ABPI) or ankle-brachial index (ABI) is the ratio of the blood pressure at the ankle to the blood pressure in the upper arm (brachium). Compared to the arm, lower blood pressure in the leg suggests blocked arteries due to peripheral artery disease (PAD). The ABPI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure in the arm.

Capillary refill time (CRT) is defined as the time taken for color to return to an external capillary bed after pressure is applied to cause blanching. It can be measured by holding a hand higher than heart-level and pressing the soft pad of a finger or fingernail until it turns white, then taking note of the time needed for the color to return once pressure is released. In humans, CRT of more than three seconds indicates decreased peripheral perfusion and may indicate cardiovascular or respiratory dysfunction. The most reliable and applicable site for CRT testing is the finger pulp, and the cut-off value for the normal CRT should be 3 seconds, not 2 seconds.
A peripheral vascular examination is a medical examination to discover signs of pathology in the peripheral vascular system. It is performed as part of a physical examination, or when a patient presents with leg pain suggestive of a cardiovascular pathology.
A vascular bypass is a surgical procedure performed to redirect blood flow from one area to another by reconnecting blood vessels. Often, this is done to bypass around a diseased artery, from an area of normal blood flow to another relatively normal area. It is commonly performed due to inadequate blood flow (ischemia) caused by atherosclerosis, as a part of organ transplantation, or for vascular access in hemodialysis. In general, someone's own vein (autograft) is the preferred graft material for a vascular bypass, but other types of grafts such as polytetrafluoroethylene (Teflon), polyethylene terephthalate (Dacron), or a different person's vein (allograft) are also commonly used. Arteries can also serve as vascular grafts. A surgeon sews the graft to the source and target vessels by hand using surgical suture, creating a surgical anastomosis.
Lisker's sign is a clinical sign in which there is tenderness when the front, middle (anteromedial) part of the tibia is percussed. It can be found in people who have deep venous thrombosis.
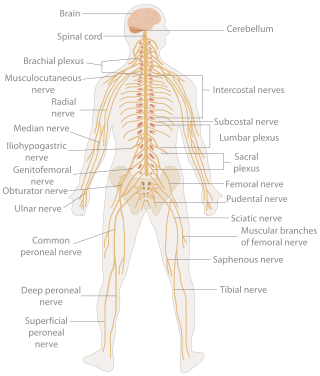
A neurological examination is the assessment of sensory neuron and motor responses, especially reflexes, to determine whether the nervous system is impaired. This typically includes a physical examination and a review of the patient's medical history, but not deeper investigation such as neuroimaging. It can be used both as a screening tool and as an investigative tool, the former of which when examining the patient when there is no expected neurological deficit and the latter of which when examining a patient where you do expect to find abnormalities. If a problem is found either in an investigative or screening process, then further tests can be carried out to focus on a particular aspect of the nervous system.

Vascular disease is a class of diseases of the vessels of the circulatory system in the body, including blood vessels – the arteries and veins, and the lymphatic vessels. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood and lymph vessels can cause a range of health problems that can sometimes become severe, and fatal. Coronary heart disease for example, is the leading cause of death for men and women in the United States.

Acrocyanosis is persistent blue or cyanotic discoloration of the extremities, most commonly occurring in the hands, although it also occurs in the feet and distal parts of face. Although described over 100 years ago and not uncommon in practice, the nature of this phenomenon is still uncertain. The very term "acrocyanosis" is often applied inappropriately in cases when blue discoloration of the hands, feet, or parts of the face is noted. The principal (primary) form of acrocyanosis is that of a benign cosmetic condition, sometimes caused by a relatively benign neurohormonal disorder. Regardless of its cause, the benign form typically does not require medical treatment. A medical emergency would ensue if the extremities experience prolonged periods of exposure to the cold, particularly in children and patients with poor general health. However, frostbite differs from acrocyanosis because pain often accompanies the former condition, while the latter is very rarely associated with pain. There are also a number of other conditions that affect hands, feet, and parts of the face with associated skin color changes that need to be differentiated from acrocyanosis: Raynaud phenomenon, pernio, acrorygosis, erythromelalgia, and blue finger syndrome. The diagnosis may be challenging in some cases, especially when these syndromes co-exist.

Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein. The most common cause of CVI is superficial venous reflux which is a treatable condition. As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.
Buerger's test is performed in an assessment of arterial sufficiency. It is named after Leo Buerger. The vascular angle, which is also called Buerger's angle, is the angle to which the leg has to be raised before it becomes pale, whilst lying down. In a limb with a normal circulation the toes and sole of the foot, stay pink, even when the limb is raised by 90 degrees. In an ischaemic leg, elevation to 15 degrees or 30 degrees for 30 to 60 seconds may cause pallor. A vascular angle of less than 20 degrees indicates severe ischaemia.
Bancroft's sign, also known as Moses' sign, is a clinical sign found in patients with deep vein thrombosis of the lower leg involving the posterior tibial veins. The sign is positive if pain is elicited when the calf muscle is compressed forwards against the tibia, but not when the calf muscle is compressed from side to side. Like other clinical signs for deep vein thrombosis, such as Homans sign and Lowenberg's sign, this sign is neither sensitive nor specific for the presence of thrombosis.
Lowenberg's sign is a clinical sign found in patients with deep vein thrombosis of the lower leg. The sign is positive when pain is elicited rapidly when a blood pressure cuff is placed around the calf and inflated to 80mmHg. Like other signs of deep vein thrombosis, such as Homans sign and Bancroft's sign, this sign is neither sensitive nor specific for the presence of thrombosis.
Louvel's sign is a clinical sign found in patients with deep vein thrombosis. The sign is defined as pain in the distribution of the affected vein which occurs during coughing or sneezing, and which disappears when the vein is compressed proximally.
Chronic limb threatening ischemia (CLTI), also known as critical limb ischemia (CLI), is an advanced stage of peripheral artery disease (PAD). It is defined as ischemic rest pain, arterial insufficiency ulcers, and gangrene. The latter two conditions are jointly referred to as tissue loss, reflecting the development of surface damage to the limb tissue due to the most severe stage of ischemia. Compared to the other manifestation of PAD, intermittent claudication, CLI has a negative prognosis within a year after the initial diagnosis, with 1-year amputation rates of approximately 12% and mortality of 50% at 5 years and 70% at 10 years.
Rajiv Parakh is the chairman at the Division of Peripheral Vascular and Endovascular Sciences at Medanta, Gurgaon, India. In 1986 he completed his vascular surgery training and acquired a fellowship from the Royal College of Surgeons in the United Kingdom. He returned to India where, in 1990, he established one of the country's first independent departments of vascular surgery at a city hospital.
Sickle cell retinopathy can be defined as retinal changes due to blood vessel damage in the eye of a person with a background of sickle cell disease. It can likely progress to loss of vision in late stages due to vitreous hemorrhage or retinal detachment. Sickle cell disease is a structural red blood cell disorder leading to consequences in multiple systems. It is characterized by chronic red blood cell destruction, vascular injury, and tissue ischemia causing damage to the brain, eyes, heart, lungs, kidneys, spleen, and musculoskeletal system.
References
- ↑ Williams, Mark E (2008). "Chapter 18. The peripheral vascular examination". Geriatric physical diagnosis: a guide to observation and assessment. McFarland & Company Inc. p. 221. ISBN 978-0-7864-3009-3.
- ↑ Assessment of the Elderly Patient: The Peripheral Vascular Examination: Venous Examinations at Medscape.