Aortic stenosis is the narrowing of the exit of the left ventricle of the heart, such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse over time. Symptoms often come on gradually with a decreased ability to exercise often occurring first. If heart failure, loss of consciousness, or heart related chest pain occur due to AS the outcomes are worse. Loss of consciousness typically occurs with standing or exercising. Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs. Thickening of the valve without narrowing is known as aortic sclerosis.

A heart valve is a one-way valve that normally allows blood to flow in only one direction through the heart. The four valves are commonly represented in a mammalian heart that determines the pathway of blood flow through the heart. A heart valve opens or closes incumbent on differential blood pressure on each side.

Heart sounds are the noises generated by the beating heart and the resultant flow of blood through it. Specifically, the sounds reflect the turbulence created when the heart valves snap shut. In cardiac auscultation, an examiner may use a stethoscope to listen for these unique and distinct sounds that provide important auditory data regarding the condition of the heart.

The aortic valve is a valve in the human heart between the left ventricle and the aorta. It is one of the two semilunar valves of the heart, the other being the pulmonary valve. The heart has four valves; the other two are the mitral and the tricuspid valves. The aortic valve normally has three cusps or leaflets, although in 1–2% of the population it is found to congenitally have two leaflets. The aortic valve is the last structure in the heart the blood travels through before stopping the flow through the systemic circulation.

Heart murmurs are heart sounds produced when blood is pumped across a heart valve and creates a sound loud enough to be heard with a stethoscope. Murmurs are of various types and are important in the detection of cardiac and valvular pathologies.

The systole is the part of the cardiac cycle during which some chambers of the heart muscle contract after refilling with blood. The term originates, via New Latin, from Ancient Greek συστολή (sustolē), from συστέλλειν, and is similar to the use of the English term to squeeze.

A ventricle is one of two large chambers toward the bottom of the heart that collect and expel blood received from an atrium towards the peripheral beds within the body and lungs. The atrium primes the pump.

Afterload is the pressure that the heart must work against to eject blood during systole. Afterload is proportional to the average arterial pressure. As aortic and pulmonary pressures increase, the afterload increases on the left and right ventricles respectively. Afterload changes to adapt to the continually changing demands on an animal's cardiovascular system. Afterload is proportional to mean systolic blood pressure and is measured in millimeters of mercury.

The pulmonary valve is the semilunar valve of the heart that lies between the right ventricle and the pulmonary artery and has three cusps. Similar to the aortic valve, the pulmonary valve opens in ventricular systole, when the pressure in the right ventricle rises above the pressure in the pulmonary artery. At the end of ventricular systole, when the pressure in the right ventricle falls rapidly, the pressure in the pulmonary artery will close the pulmonary valve.

Mitral stenosis is a valvular heart disease characterized by the narrowing of the orifice of the mitral valve of the heart. It is almost always caused by rheumatic valvular heart disease. Normally, the mitral valve is about 5 cm2 during diastole. Any decrease in area below 2 cm2 causes mitral stenosis. Early diagnosis of mitral stenosis in pregnancy is very important as the heart cannot tolerate increased cardiac output demand as in the case of exercise and pregnancy. Atrial fibrillation is a common complication of resulting left atrial enlargement, which can lead to systemic thromboembolic complications like stroke.
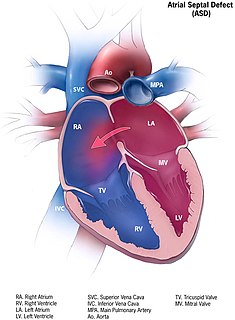
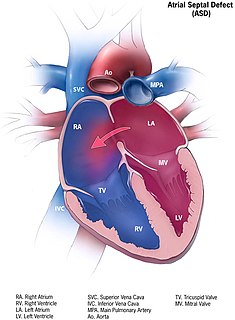
Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this does not naturally close after birth it is referred to as a patent (open) foramen ovale (PFO). It is common in patients with a congenital atrial septal aneurysm (ASA).

A ventricular septal defect (VSD) is a defect in the ventricular septum, the wall dividing the left and right ventricles of the heart. The extent of the opening may vary from pin size to complete absence of the ventricular septum, creating one common ventricle. The ventricular septum consists of an inferior muscular and superior membranous portion and is extensively innervated with conducting cardiomyocytes.
A transthoracic echocardiogram (TTE) is the most common type of echocardiogram, which is a still or moving image of the internal parts of the heart using ultrasound. In this case, the probe is placed on the chest or abdomen of the subject to get various views of the heart. It is used as a non-invasive assessment of the overall health of the heart, including a patient's heart valves and degree of heart muscle contraction. The images are displayed on a monitor for real-time viewing and then recorded.

The cardiac cycle is the performance of the human heart from the beginning of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, following a period of robust contraction and pumping of blood, dubbed systole. After emptying, the heart immediately relaxes and expands to receive another influx of blood returning from the lungs and other systems of the body, before again contracting to pump blood to the lungs and those systems. A normally performing heart must be fully expanded before it can efficiently pump again. Assuming a healthy heart and a typical rate of 70 to 75 beats per minute, each cardiac cycle, or heartbeat, takes about 0.8 seconds to complete the cycle. There are two atrial and two ventricle chambers of the heart; they are paired as the left heart and the right heart—that is, the left atrium with the left ventricle, the right atrium with the right ventricle—and they work in concert to repeat the cardiac cycle continuously,. At the start of the cycle, during ventricular diastole–early, the heart relaxes and expands while receiving blood into both ventricles through both atria; then, near the end of ventricular diastole–late, the two atria begin to contract, and each atrium pumps blood into the ventricle below it. During ventricular systole the ventricles are contracting and vigorously pulsing two separated blood supplies from the heart—one to the lungs and one to all other body organs and systems—while the two atria are relaxed. This precise coordination ensures that blood is efficiently collected and circulated throughout the body.

Valvular heart disease is any cardiovascular disease process involving one or more of the four valves of the heart. These conditions occur largely as a consequence of aging, but may also be the result of congenital (inborn) abnormalities or specific disease or physiologic processes including rheumatic heart disease and pregnancy.

Pulmonary valve stenosis (PVS) is a heart valve disorder. Blood going from the heart to the lungs goes through the pulmonary valve, whose purpose is to prevent blood from flowing back to the heart. In pulmonary valve stenosis this opening is too narrow, leading to a reduction of flow of blood to the lungs.
Pulmonic stenosis, is a dynamic or fixed obstruction of flow from the right ventricle of the heart to the pulmonary artery. It is usually first diagnosed in childhood.
A right-to-left shunt is a cardiac shunt which allows blood to flow from the right heart to the left heart. This terminology is used both for the abnormal state in humans and for normal physiological shunts in reptiles.

Lutembacher's syndrome is a very rare form of congenital heart disease that affects one of the chambers of the heart as well as a valve. It is commonly known as both congenital atrial septal defect (ASD) and acquired mitral stenosis (MS). Congenital atrial septal defect refers to a hole being in the septum or wall that separates the two atria; this condition is usually seen in fetuses and infants. Mitral stenosis refers to mitral valve leaflets sticking to each other making the opening for blood to pass from the atrium to the ventricles very small. With the valve being so small, blood has difficulty passing from the left atrium into the left ventricle. Septal defects that may occur with Lutembacher's syndrome include: Ostium primum atrial septal defect or ostium secundum which is more prevalent.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.