The history of tuberous sclerosis (TSC) research spans less than 200 years. TSC is a rare, multi-system genetic disease that can cause benign tumours to grow on the brain or other vital organs such as the kidneys, heart, eyes, lungs, and skin. A combination of symptoms may include seizures, developmental delay, behavioural problems and skin abnormalities, as well as lung and kidney disease. TSC is caused by mutations on either of two genes, TSC1 and TSC2, which encode for the proteins hamartin and tuberin respectively. These proteins act as tumour growth suppressors and regulate cell proliferation and differentiation. [1] Originally regarded as a rare pathological curiosity, it is now an important focus of research into tumour formation and suppression.
Contents
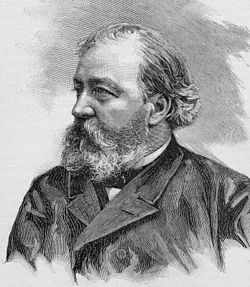
The history of TSC research is commonly divided into four periods. [2] In the late 19th century, notable physicians working in European teaching hospitals first described the cortical and dermatological manifestations; these early researchers have been awarded with eponyms such as "Bourneville's disease" [3] and "Pringle's adenoma sebaceum". [4] At the start of the 20th century, these symptoms were recognised as belonging to a single medical condition. Further organ involvement was discovered, along with a realisation that the condition was highly variable in its severity. The late 20th century saw great improvements in cranial imaging techniques and the discovery of the two genes. Finally, the start of the 21st century saw the beginning of a molecular understanding of the illness, along with possible non-surgical therapeutic treatments.







