Cardiac arrest, also known as sudden cardiac arrest, is when the heart suddenly and unexpectedly stops beating. As a result, blood cannot properly circulate around the body and there is diminished blood flow to the brain and other organs. When the brain does not receive enough blood, this can cause a person to pass out and become unresponsive. Cardiac arrest is also identified by a lack of central pulses and abnormal or absent breathing.

Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation, or mouth to mouth in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person who is in cardiac arrest. It is recommended for those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.

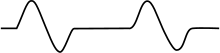
Asystole is the absence of ventricular contractions in the context of a lethal heart arrhythmia. Asystole is the most serious form of cardiac arrest and is usually irreversible. Also referred to as cardiac flatline, asystole is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.
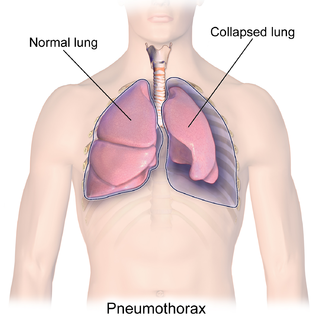
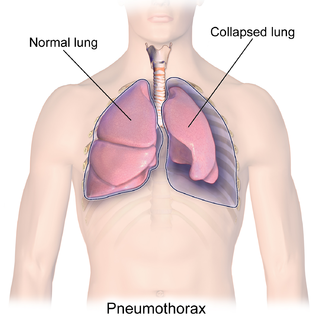
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed by an area of damaged tissue, and the amount of air in the space between chest wall and lungs increases; this is called a tension pneumothorax. This can cause a steadily worsening oxygen shortage and low blood pressure. This leads to a type of shock called obstructive shock, which can be fatal unless reversed. Very rarely, both lungs may be affected by a pneumothorax. It is often called a "collapsed lung", although that term may also refer to atelectasis.

Internal bleeding is a loss of blood from a blood vessel that collects inside the body, and is not usually visible from the outside. It can be a serious medical emergency but the extent of severity depends on bleeding rate and location of the bleeding. Severe internal bleeding into the chest, abdomen, pelvis, or thighs can cause hemorrhagic shock or death if proper medical treatment is not received quickly. Internal bleeding is a medical emergency and should be treated immediately by medical professionals.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.

Advanced Life Support (ALS) is a set of life saving protocols and skills that extend basic life support to further support the circulation and provide an open airway and adequate ventilation (breathing).

A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to Pneumothorax, or rarely in association with other conditions.

ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, sports-related injuries, and are notably common among the elderly who experience falls.

A chest injury, also known as chest trauma, is any form of physical injury to the chest including the ribs, heart and lungs. Chest injuries account for 25% of all deaths from traumatic injury. Typically chest injuries are caused by blunt mechanisms such as direct, indirect, compression, contusion, deceleration, or blasts caused by motor vehicle collisions or penetrating mechanisms such as stabbings.

The AutoPulse is an automated, portable, battery-powered cardiopulmonary resuscitation device created by Revivant and subsequently purchased and currently manufactured by ZOLL Medical Corporation. It is a chest compression device composed of a constricting band and half backboard that is intended to be used as an adjunct to CPR during advanced cardiac life support by professional health care providers. The AutoPulse uses a distributing band to deliver the chest compressions. In literature it is also known as LDB-CPR.
A gunshot wound (GSW) is a penetrating injury caused by a projectile from a gun. Damages may include bleeding, bone fractures, organ damage, wound infection, loss of the ability to move part of the body, and in severe cases, death. Damage depends on the part of the body hit, the path the bullet follows through the body, and the type and speed of the bullet. Long-term complications can include bowel obstruction, failure to thrive, neurogenic bladder and paralysis, recurrent cardiorespiratory distress and pneumothorax, hypoxic brain injury leading to early dementia, amputations, chronic pain and pain with light touch (hyperalgesia), deep venous thrombosis with pulmonary embolus, limb swelling and debility, and lead poisoning.
The Arctic Sun Temperature Management System is a non-invasive targeted temperature management system. It modulates patient temperature by circulating chilled water in pads directly adhered to the patient's skin. Using varying water temperatures and a computer algorithm, a patient's body temperature can be better controlled. It is produced by Medivance, Inc. of Louisville, Colorado.
The Hs and Ts is a mnemonic used to aid in remembering the possible reversible causes of cardiac arrest. A variety of disease processes can lead to a cardiac arrest; however, they usually boil down to one or more of the "Hs and Ts".
A transmediastinal gunshot wound (TMGSW) is a penetrating injury to a person's thorax in which a bullet enters the mediastinum, possibly damaging some of the major structures in this area. Hemodynamic instability has been reported in about 50% of cases with a mortality rate ranging from 20% to 49%. Some studies have shown marked improvement in the mortality rate of patients who survived transfer to the operating room rather than being treated surgically in the ER.

A resuscitative thoracotomy (sometimes referred to as an emergency department thoracotomy (EDT), trauma thoracotomy or, colloquially, as "cracking the chest") is a thoracotomy performed to aid in the resuscitation of a major trauma patient who has sustained severe thoracic or abdominal trauma. The procedure allows immediate direct access to the thoracic cavity, permitting rescuers to control hemorrhage, relieve cardiac tamponade, repair or control major injuries to the heart, lungs or thoracic vasculature, and perform direct cardiac massage or defibrillation. The procedure is rarely performed and is a procedure of last resort.
Extracorporeal cardiopulmonary resuscitation is a method of cardiopulmonary resuscitation (CPR) that passes the patient's blood through a machine in a process to oxygenate the blood supply. A portable extracorporeal membrane oxygenation (ECMO) device is used as an adjunct to standard CPR. A patient who is deemed to be in cardiac arrest refractory to CPR has percutaneous catheters inserted into the femoral vein and artery. Theoretically, the application of ECPR allows for the return of cerebral perfusion in a more sustainable manner than with external compressions alone. By attaching an ECMO device to a person who has acutely undergone cardiovascular collapse, practitioners can maintain end-organ perfusion whilst assessing the potential reversal of causal pathology, with the goal of improving long-term survival and neurological outcomes.

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a minimally invasive procedure performed during resuscitation of critically injured trauma patients. Originally developed as a less invasive alternative to emergency thoracotomy with aortic cross clamping, REBOA is performed to gain rapid control of non-compressible truncal or junctional hemorrhage. REBOA is performed first by achieving access to the common femoral artery (CFA) and advancing a catheter within the aorta. Upon successful catheter placement, an occluding balloon may be inflated either within the descending thoracic aorta or infrarenal abdominal aorta. REBOA stanches downstream hemorrhage and improves cardiac index, cerebral perfusion, and coronary perfusion. Although REBOA does not eliminate the need for definitive hemorrhage control, it may serve as a temporizing measure during initial resuscitation. Despite the benefits of REBOA, there are significant local and systemic ischemic risks. Establishing standardized REBOA procedural indications and mitigating the risk of ischemic injury are topics of ongoing investigation. Although this technique has been successfully deployed in adult patients, it has not yet been studied in children.