Nervous system
| | This section is empty. You can help by adding to it. (February 2020) |
Oral manifestations of systematic disease are signs and symptoms of disease occurring elsewhere in the body detected in the oral cavity and oral secretions. High blood sugar can be detected by sampling saliva. [1] Saliva sampling may be a non-invasive way to detect changes in the gut microbiome and changes in systemic disease. Another example is tertiary syphilis, where changes to teeth can occur. [2] Syphilis infection can be associated with longitudinal furrows of the tongue.
Mineral and vitamin deficiencies can cause the tongue to appear beefy red and feel sore. Those deficiencies are iron, folate, and vitamin B12. A hairy tongue may be an indication of Epstein Barr virus infection and is usually seen in those infected with human immunodeficiency virus. Other systemic diseases that can cause the tongue to form aphthous ulcers are: Crohn's disease and ulcerative colitis, Behcet's Syndrome, pemphigus vulgaris, herpes simplex, histoplasmosis, and reactive arthritis. [3]
A heart attack is a blood vessel in the heart being constricted either by a blood clot or atherosclerosis formation. A heart attack can cause pain the chest; sometimes this pain can radiate up to the jaw. (Malik et al., 2013) [4]
Calcium channel blockers are medications prescribed for the treatment of a number of heart conditions and primarily to treat high blood pressure. They can cause gingival hypertrophy (overgrowth), particularly dihydropyridine and nifidipine. Poor dental hygiene and inflamed gums are a risk factor. The overgrowth is not permanent, it is suggested that if the medication is stopped then the overgrowth can reduce[ however, this is a decision that would have to be made in conjunction with the patient's dentist and cardiologist as the risk of stopping some medications outweigh any advantage gained (Livada and Shiloah, 2013) [5]
Nicorandil is a medication that is prescribed for the treatment of angina. It can cause major aphthous-like ulcer formation (BNF, 2020). [6]
Iron, folate and vitamin B12 deficiencies – The most commonest cause of iron deficiencies is low ferritin; this can cause the tongue to appear beefy red and appear sore. It can also present in the mouth as angular chelitis, which is an infection caused by either staphylococcus or candidiasis, and can make the corners of the mouth appear red and crispy.
Sickle cell disease is a hereditary genetic condition that results in deformed red blood cells to be formed. Sickle patients can experience sickle crisis, these are painful events in which if in the jaw can mimic dental pain and facial swelling can also occur during a crisis. The dental pulp can be affected by sickling and there may be a delayed eruption and hypoplasia of the dentition. Sickle patients are also at an increased risk of developing infection.
Thalasseamias is a group of inherited genetic disorders that affect the haemoglobin synthesis; it can result in either a reduced or absent globin chain production. If beta thalassaemia major is left untreated or under transfused, there is expansion of ineffective bone marrow, this leads to bony deformities resulting in dental malocclusion. Beta thalassaemia major patients may also be on bisphosphonates and are therefore at risk of developing osteonecrosis of the jaw.
Thrombocytopenia is a deficiency of platelets in the blood. It can present as red blood blisters in the mouth.
Patients with respiratory conditions like asthma and chronic obstructive pulmonary disease can be prescribed steroidal inhalers to help strengthen their lungs. They must ensure after use that they rinse their mouths, otherwise there is an increase of dental caries, xerostomia, candidiasis, ulceration and gingivitis/periodontitis (Godara et al., 2011). [7]
There are a number of oral complications following renal transplantation. Ciclosporin is an immunosuppressant medication that is used to help prevent patients from rejecting the transplanted kidney (BNF, 2020). Due to the immunosuppression (suppressed immune system), these patients are more likely to have gingival hyperplasia, aphthous ulceration, herpes simplex virus, oral leucoplakia; which may transform into squamous cell carcinoma, candidiasis infection or Kaposi's sarcoma (BNF, 2020). [6]
There are many specific diseases of the gastrointestinal tract which have an impact on oral health. Systemic disease can affect the upper GI tract such as dysphagia, dysmotility, gastro-oesophageal reflux and peptic ulcer disease; or lower in the tract such as coeliac disease, Crohn's disease, ulcerative colitis and familial adenomatous polyposis. [8]
Dysphagia is defined as a difficulty in swallowing. Structurally it worsens when eating solids and neurologically it is worse with fluids. [9] Structural problems may include malignancy, stricture and pharyngeal pouching which can lead to halitosis, regurgitation of undigested food and high feeling of dysphagia. Neurological problems may be related to the patient having multiple sclerosis, motor neuron disease, or having had a stroke. [10] Dysphagia may present as a barrier to care in the dental setting as the patient may require high volume suction in order to maintain patient comfort and reduce the risk of aspiration of dental material/ fluids.
Gastroesophageal reflux can present as retrosternal pain, acid brash and a hoarse voice. Risk factors for gastroesophageal reflux disease are obesity, diet, smoking and hiatal hernia. Complications of which being oesophagitis, Barrett's oesophagus, Strictures and ulcers. Common management of gastroesophageal reflux disease include lifestyle measures, proton pump inhibitors and rarely surgery. There is a clear relationship between gastroesophageal reflux disease and dental erosion and therefore can be detrimental to hard tissues i.e. teeth and also soft tissues of the mouth. [11]
Crohn's disease is a patchy disease which can affect any area of the GI tract from the oral cavity to the anus. The manifestations depend on the affected area. The oral manifestations present as orofacial granulomatosis, an inflammatory condition affecting the oral mucosa. It is non-caveating granulomas and has a "cobblestone" appearance. Orofacial granulomatosis can be isolated or a manifestation of Crohn's disease and can be treated with local or systemic corticosteroids. An aggravating factor is cinnamon, therefore a cinnamon-free diet is recommended. [8]
Eating disorders are a psychological problem which has an impact on the gastrointestinal tract. Two common eating disorders are anorexia nervosa and bulimia nervosa. Anorexia nervosa is a refusal to maintain a "normal" body weight with a fear of weight gain and distorted perception of body image. Bulimia nervosa is binge-eating followed by attempts to restrict weight gain and can include purging. Eating disorder oral manifestation is severe palatal erosion due to vomiting. There is occlusal erosion of the maxillary teeth causing the incised edges of the incisors to be thin and knife-edged. Occlusal surfaces have a flat to cupped-out appearance. [12] Extra-orally eating disorders may present with swollen parotid glands.
Other oral manifestations of GI disease is angular stomatitis, commonly seen in iron-deficient anaemia and mouth ulcers in Crohn's disease.
Diabetes Mellitus has two main types: Type 1, autoimmune destruction of beta-cells leading to reduced insulin production and Type 2, the body becomes increasingly resistant to the effects of insulin leading to the bodies inability to regulate plasma glucose levels resulting in a fall in insulin production. Diabetes has numerous implications on oral health. Patient with diabetes have increase extent and severity of periodontal disease, increased prevalence of dental caries due to xerostomia, can experience burning mouth syndrome and candidal infections as well as experiencing altered taste sensation, altered tooth eruption and hypertrophy of the parotid glands. Other oral health problems include chronic hyperglycaemia, infection, delayed wound healing and lichen planus/lichenoid reactions. [13]
The oral manifestations of Acromegaly predominate as spacing of the lower incisor teeth and widening of the mandible. Other complications include visual field defects, headaches, Diabetes, Sleep apnoea, Hypertension, Arthralgia and Arthritis and Carpal Tunnel Syndrome. [13] Arthralgia and Carpal Tunnel Syndrome both have an impact on a patients' ability to maintain good oral hygiene practice and therefore may predispose them to Dental caries and Periodontal Disease. It is imperative these patients are given Enhanced Prevention in order to reduce the risk of Dental Caries and Periodontal Disease.
Another endocrine disorder that may present orally is Addison's disease. Signs include skin hyperpigmentation, alabaster-coloured pale skin, low blood pressure, postural hypotension. Skin pigmentation have increased deposition in the palmer skin creases, nails and gingiva. [13] Management of Addison's is with steroids. During dental treatment the patient may require an increased dose of steroids based on treatment need.
Osteopgenesis imperfecta, also known as brittle bone disease, is caused by a gene mutation affecting the collagen genes, patients generally present with a large number of fractures from minor injuries. Teeth, if affected, are of the appearance of dentinogenesis imperfecta.
Osteoporosis is a very common disease associated with a decreased bone mineral density, it mainly affects post menopausal women whose oestrogen levels have dropped. It is managed with the used of bisphosphonates. Prior to placement on bisphosphonates, a dental check must be done to extract any hopeless teeth as extractions in patients who have prolonged used of bisphosphonates are at risk of MRONJ.[ clarification needed ] (SDCEP,2017)
Human immunodeficiency virus infects and destroys cells of the immune system, principally the CD4+ T-helper lymphocytes. As well as lymphocytes, CD4 receptors are also present on the surface of macrophages and monocytes, cells in the brain, skin, and probably many other sites. The normal CD4 count is 500-1500 per mm3, and patients with human immunodeficiency virus infection often have a CD4 count less than 500. Patients who are infected with human immunodeficiency virus positive have an increased risk of developing infections and tumours. The lower the CD4 count, the greater the likelihood and the severity of illness. A CD4 count less than 200 is a diagnosis of Acquired Immunodeficiency Syndrome (AIDS). Oral manifestations of human immunodeficiency virus include candidiasis, oral hairy leukoplakia, oral ulcers, oral warts, oral lymphoma and Kaposi's sarcoma. [13] Other presentations include gingivitis and oral malignancies. Treatment and management of AIDS is based on highly active anti-retroviral therapy, which significantly lowers the prevalence of oral lesions, particularly oral candidiasis and oral hairy leukoplakia. [14]
| | This section is empty. You can help by adding to it. (February 2020) |
| | This section is empty. You can help by adding to it. (February 2020) |

Candidiasis is a fungal infection due to any type of Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers along with other symptoms depending on the parts involved.

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is one of the upper gastrointestinal chronic diseases in which stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. In the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.

Esophagitis, also spelled oesophagitis, is a disease characterized by inflammation of the esophagus. The esophagus is a tube composed of a mucosal lining, and longitudinal and circular smooth muscle fibers. It connects the pharynx to the stomach; swallowed food and liquids normally pass through it.

A mouth ulcer (aphtha) is an ulcer that occurs on the mucous membrane of the oral cavity. Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying cause. Rarely, a mouth ulcer that does not heal may be a sign of oral cancer. These ulcers may form individually or multiple ulcers may appear at once. Once formed, an ulcer may be maintained by inflammation and/or secondary infection.

Uremia is the term for high levels of urea in the blood. Urea is one of the primary components of urine. It can be defined as an excess in the blood of amino acid and protein metabolism end products, such as urea and creatinine, which would be normally excreted in the urine. Uremic syndrome can be defined as the terminal clinical manifestation of kidney failure. It is the signs, symptoms and results from laboratory tests which result from inadequate excretory, regulatory, and endocrine function of the kidneys. Both uremia and uremic syndrome have been used interchangeably to denote a very high plasma urea concentration that is the result of renal failure. The former denotation will be used for the rest of the article.

An upper gastrointestinal series, also called a barium swallow, barium study, or barium meal, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into "barium swallow", "barium meal", "barium follow-through", and "enteroclysis". To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called "CT enterography".
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that affect the patient's immune system. Examples of these extrinsic factors include HIV infection and environmental factors, such as nutrition. Immunocompromisation may also be due to genetic diseases/flaws such as SCID.

A feeding tube is a medical device used to provide nutrition to people who cannot obtain nutrition by mouth, are unable to swallow safely, or need nutritional supplementation. The state of being fed by a feeding tube is called gavage, enteral feeding or tube feeding. Placement may be temporary for the treatment of acute conditions or lifelong in the case of chronic disabilities. A variety of feeding tubes are used in medical practice. They are usually made of polyurethane or silicone. The diameter of a feeding tube is measured in French units. They are classified by the site of insertion and intended use.
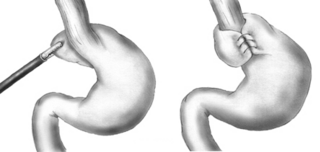
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Xerostomia, also known as dry mouth, is dryness in the mouth, which may be associated with a change in the composition of saliva, or reduced salivary flow, or have no identifiable cause.

Glossitis can mean soreness of the tongue, or more usually inflammation with depapillation of the dorsal surface of the tongue, leaving a smooth and erythematous (reddened) surface,. In a wider sense, glossitis can mean inflammation of the tongue generally. Glossitis is often caused by nutritional deficiencies and may be painless or cause discomfort. Glossitis usually responds well to treatment if the cause is identified and corrected. Tongue soreness caused by glossitis is differentiated from burning mouth syndrome, where there is no identifiable change in the appearance of the tongue, and there are no identifiable causes.
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use. The oral mucosa tends to heal faster and with less scar formation compared to the skin. The underlying mechanism remains unknown, but research suggests that extracellular vesicles might be involved.
An oral medicine or stomatology doctor/dentist has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region, essentially as a "physician of the mouth".

Oropharyngeal dysphagia is the inability to empty material from the oropharynx into the esophagus as a result of malfunction near the esophagus. Oropharyngeal dysphagia manifests differently depending on the underlying pathology and the nature of the symptoms. Patients with dysphagia can experience feelings of food sticking to their throats, coughing and choking, weight loss, recurring chest infections, or regurgitation. Depending on the underlying cause, age, and environment, dysphagia prevalence varies. In research including the general population, the estimated frequency of oropharyngeal dysphagia has ranged from 2 to 16 percent.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.
Osteonecrosis of the jaw (ONJ) is a severe bone disease (osteonecrosis) that affects the jaws. Various forms of ONJ have been described since 1861, and a number of causes have been suggested in the literature.
Osteomyelitis of the jaws is osteomyelitis which occurs in the bones of the jaws. Historically, osteomyelitis of the jaws was a common complication of odontogenic infection. Before the antibiotic era, it was frequently a fatal condition.
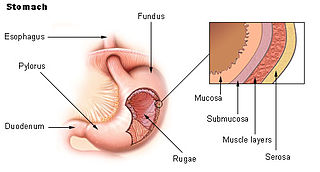
Acid peptic diseases, such as peptic ulcers, Zollinger-Ellison syndrome, and gastroesophageal reflux disease, are caused by distinct but overlapping pathogenic mechanisms involving acid effects on mucosal defense. Acid reflux damages the esophageal mucosa and may also cause laryngeal tissue injury, leading to the development of pulmonary symptoms.
{{cite web}}: CS1 maint: archived copy as title (link)