| Hereditary gingival fibromatosis | |
|---|---|
| Other names | Autosomal dominant gingival hyperplasia, idiopathic gingival hyperplasia |
| Specialty | Dentistry |
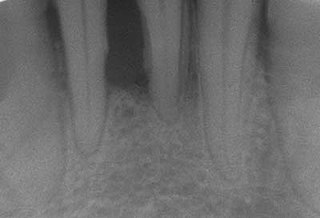
Hereditary gingival fibromatosis (HGF), also known as idiopathic gingival hyperplasia, is a rare condition of gingival overgrowth. [1] HGF is characterized as a benign, slowly progressive, nonhemorrhagic, fibrous enlargement of keratinized gingiva. It can cover teeth in various degrees, and can lead to aesthetic disfigurement. [2] Fibrous enlargement is most common in areas of maxillary and mandibular tissues of both arches in the mouth. [1] Phenotype and genotype frequency of HGF is 1:175,000 where males and females are equally affected but the cause is not entirely known. [2] [3] It mainly exists as an isolated abnormality but can also be associated with a multi-system syndrome. [1]
There may or may not be any evidence of history of HGF in the family nor any usage of taking long-term medicines for any particular disease when it comes to diagnosing HGF. There also may or may not be any signs of medical and/or family history of mental retardation, hypertrichosis, nor clinical symptoms that can be associated with gingival enlargement. Although, enlargement of gingiva, interdental papilla, hindered speech, and secondary inflammatory changes taking place in the mouth commonly at the marginal gingiva are all very indicative of this condition. Commonly the patient will have mandibular and maxilliary inflammation and overgrowth as opposed to the traditional pink, firm, and fleshy consistency of healthy gingiva. The patient's jaw may also appear distorted because of the gingiva enlargements. Overgrowth of the gingiva can range from slightly covering the surface of teeth or it can even completely cover the surrounding teeth. The patient can also experience damage or loss of teeth. [1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12]
Though much more research needs to be done, researchers have mostly agreed that a mutation in SOS1, son-of-sevenless gene, is responsible for this disease. [1] [4] [5] [6] SOS1 is a guanine nucleotide-exchange factor that functions in the transduction of signals that control cell growth and differentiation. A mutation in the SOS1 gene results in a single nucleotide insertion. [6] Specific linkage studies have localized the mutation for isolated, nonsyndromic autosomal dominant forms of gingival fibromatosis to chromosomes 2 and 5, more specifically 2p21-p22 and 5q13-q22. [1]
HGF1 - Caused by a mutation in the SOS1 gene localized on chromosome 2p21-p22 [1]
HGF2 - Caused by a mutation in the SOS1 gene localized on chromosome 5q13-q22 [1] [ contradictory ]
Mutations in the RE1-silencing transcription factor (REST) gene can also cause this syndrome. [13]
HGF may also be caused by unwanted side effects of pharmacological agents like phenytoin, ciclosporin, and some calcium-channel blockers, meaning HGF is a disease that can be drug-induced. [1] However, there is little next to no research done in this area to support the claim.
Genetic linkage studies are among the most popular methods of study to look at the mechanism of this HGF. Genetic linkage studies have found to localize genetic loci for autosomal dominant forms of HGF to chromosome 2p21-p22 (indicative of HGF1) and chromosome 5q13-q22 (indicative of HGF2). Chromosome 2p21-p22 has been refined to an interval of ~2.3 Mb to construct an integrated physical and genetic map of the 16 genes interval. Here, a mutation is found in sequencing these 16 genes. [2]
There is an insertion of a cytosine between nucleotides 126,142 and 126,143 in codon 1083 of the SOS1 gene, meaning there is a mutation in SOS1. This causes a problem because SOS1 introduces a frameshift mutation and creates a premature stop codon. Also, it can segregate over generations, most commonly four. Once it causes a premature stop codon, the chromosome loses four important proline-rich SH-3 binding domains in the carboxyl-terminal region of the SOS1 protein. As a result, the N-terminal amino acids for SOS1 is fused into a 22–amino acid carboxyl terminus. [2] Researchers claim that this mutation in the SOS1 gene is a probable primary cause of this disease but limited information supports the mechanism of this claim.
There are very few ways to test a patient for HGF. Currently, the most common way to diagnose a patient is by means of a physical evaluation. The physician can make a physical evaluation of the patient and send them to a dentist or better yet a specialist like a periodontist to evaluate signs of gingival overgrowth, quality of gingiva, inflammation, mechanical difficulties of the mouth, tooth conditions, and any sort of discomfort. [3]
Aside from obvious physical symptoms seen in a physical evaluation, molecular tests can be run to check if there is a mutation in the SOS1 gene to confirm the diagnosis. If there is indeed a mutation in this gene coupled with the typical physical symptoms, then it is quite probable that a patient suffers from this disease. Also, looking at family history is also becoming more prominent in aiding to diagnose the patient. Otherwise, researchers are working to find new and better ways to test for the presence of HGF. [1] [2] [9]
Since this condition is generally agreed upon to be hereditary, nothing can be done to prevent HGF. However, in some cases where it can develop as a result of rare multi-system syndromes, such as: Zimmerman-Laband, Jones, Ramon Syndrome, Rutherford Syndrome, Juvenile Hyaline Fibromatosis, Systemic Infantile Hyalinosis, and Mannosidosis, it is best for one to simply monitors the possible progression for HGF with regular dental check-ups. [8]
If the patient's disease is treated by means of surgery, it is recommended that the patient undergoes post-surgical therapies for maintenance and periodic monitoring of gums for the sake of the possibility of re-occurrence of HGF. [8]
This disease has not been shown to be life-threatening or the cause of death in patients. However, treatment is necessary to maintain a healthy lifestyle.
The following can occur if left untreated:
Most recent methods of treatment take the form of surgeries such as oral prophylaxis, followed by post-surgical therapies to monitor, provide proper oral hygiene, and correct the deformity. Although, the nature of recurrence post-treatment is virtually unknown, let alone what type of treatment is most effective for HGF. (SOURCE 2) In some cases, there is re-growth after surgical removal of the excess gingival tissues, in others there is minimal. No cases yet have shown any particular treatment or form of medicine to permanently remove HGF. [1] [2]
One type of procedure that can be executed is as follows: Removal of excess tissue under anesthesia through an internal bevel gingivectomy or undisplaced flap followed by gingivoplasty and continuous sling suture placements and periodontal dressing; after about a week of recovery after the surgery, remove sutures and periodically do observational evaluations to look for any signs of re-occurrence. [1]
Some researchers suggest that HGF is transmitted as a Mendelian trait since both autosomal dominant and autosomal recessive transmission has been reported since the early 1970s. (SOURCE 1) In more recent scientific literature, there is evidence in which pedigree analyses confirm autosomal dominant, autosomal recessive or even as X-linked inherited cases of the HGF trait. [11] [12]
In 2002, researchers described the SOS1 gene and proved for the first time that a single-nucleotide–insertion mutation of the SOS1 gene on codon 1083 is the preliminary cause of HGF1 in humans. (Source 1) Later on in 2010, there was a case study done on a 16-year-old male with severe gingival overgrowth, almost covering all teeth. Researchers approached this issue with periodontics - a partial gingivectomy and flap surgery. This case study concluded that surgery followed by regular follow-ups is a good way to treat HGF despite the fact that the risks of re-occurrence of the condition remain high. [8]
Even more recently, a study was done in 2013 on a family that showed history of autosomal recessive inheritance of HGF. The study did not dismiss the return of HGF after treatment but did claim that general surgical intervention after scaling and root planning of teeth supplemented with good oral hygiene is good enough to prevent the re-occurrence of HGF. This case study also acknowledged how HGF can be part of a multi-system syndrome associated with disorders such as Zimmermann Laband syndrome (ear, nose, bone, and nail defects with hepatosplenomegaly), Rutherford syndrome (microphthalmia, mental retardation, athetosis, and hypopigmentation), Murray-Puretic Drescher syndrome and Ramon syndrome. [1]

A genetic disorder is a health problem caused by one or more abnormalities in the genome. It can be caused by a mutation in a single gene (monogenic) or multiple genes (polygenic) or by a chromosomal abnormality. Although polygenic disorders are the most common, the term is mostly used when discussing disorders with a single genetic cause, either in a gene or chromosome. The mutation responsible can occur spontaneously before embryonic development, or it can be inherited from two parents who are carriers of a faulty gene or from a parent with the disorder. When the genetic disorder is inherited from one or both parents, it is also classified as a hereditary disease. Some disorders are caused by a mutation on the X chromosome and have X-linked inheritance. Very few disorders are inherited on the Y chromosome or mitochondrial DNA.
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen and red and may bleed. It is considered the main cause of tooth loss for adults worldwide. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or fall out. Bad breath may also occur.

The gums or gingiva consist of the mucosal tissue that lies over the mandible and maxilla inside the mouth. Gum health and disease can have an effect on general health.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.

GAPO syndrome is a rare, autosomal recessive disorder that causes severe growth retardation, and has been observed fewer than 30 times before 2011. GAPO is an acronym that encompasses the predominant traits of the disorder: growth retardation, alopecia, pseudoanodontia, and worsening optic atrophy in some subjects. Other common symptoms include premature aging, large, prominent foreheads, and delayed bone aging. GAPO syndrome typically results in premature death around age 30-40, due to interstitial fibrosis and atherosclerosis.

Zimmermann–Laband syndrome (ZLS), is an extremely rare autosomal dominant congenital disorder.
Bleeding on probing (BoP) which is also known as bleeding gums or gingival bleeding is a term used by dentists and dental hygienists when referring to bleeding that is induced by gentle manipulation of the tissue at the depth of the gingival sulcus, or interface between the gingiva and a tooth. BoP is a sign of periodontal inflammation and indicates some sort of destruction and erosion to the lining of the sulcus or the ulceration of sulcular epithelium. The blood comes from lamina propria after the ulceration of the lining. BoP seems to be correlated with Periodontal Inflamed Surface Area (PISA).

Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy or deep cleaning, is a procedure involving removal of dental plaque and calculus and then smoothing, or planing, of the (exposed) surfaces of the roots, removing cementum or dentine that is impregnated with calculus, toxins, or microorganisms, the etiologic agents that cause inflammation. It is a part of non-surgical periodontal therapy. This helps to establish a periodontium that is in remission of periodontal disease. Periodontal scalers and periodontal curettes are some of the tools involved.

Gingival enlargement is an increase in the size of the gingiva (gums). It is a common feature of gingival disease. Gingival enlargement can be caused by a number of factors, including inflammatory conditions and the side effects of certain medications. The treatment is based on the cause. A closely related term is epulis, denoting a localized tumor on the gingiva.
Gingivectomy is a dental procedure in which a dentist or oral surgeon cuts away part of the gums in the mouth.

Gingivitis is a non-destructive disease that causes inflammation of the gums. The most common form of gingivitis, and the most common form of periodontal disease overall, is in response to bacterial biofilms that is attached to tooth surfaces, termed plaque-induced gingivitis. Most forms of gingivitis are plaque-induced.

Plasma cell gingivitis is a rare condition, appearing as generalized erythema (redness) and edema (swelling) of the attached gingiva, occasionally accompanied by cheilitis or glossitis. It is called plasma cell gingivitis where the gingiva (gums) are involved, plasma cell cheilitis, where the lips are involved, and other terms such as plasma cell orifacial mucositis, or plasma cell gingivostomatitis where several sites in the mouth are involved. On the lips, the condition appears as sharply outlined, infiltrated, dark red plaque with a lacquer-like glazing of the surface of the involved oral area.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Aggressive periodontitis describes a type of periodontal disease and includes two of the seven classifications of periodontitis as defined by the 1999 classification system:
Haim–Munk syndrome is a cutaneous condition caused, like Papillon-Lefevre Syndrome, by a mutation in the cathepsin C gene. It is named after Dr. Salim Haim and Dr. J Munk, who first described the disease in 1965.

Angularis nigra, Latin for 'black angle', also known as open gingival embrasures, and colloquially known as "black triangle", is the space or gap seen at the cervical embrasure, below the contact point of some teeth. The interdental papilla does not fully enclose the space, leading to an aperture between adjacent teeth. This gap has many causes including gingival recession, and gingival withdrawal post-orthodontic work. Interdental "black triangles" were rated as the third-most-disliked aesthetic problem below caries and crown margins. Treatment of angularis nigra often requires an interdisciplinary approach, involving periodontal, orthodontic and restorative treatment. Possible treatments to correct angularis nigra include addition of composite resin in the space, veneer placement, or gum graft. Angularis nigra is generally only treated based on the aesthetic preference of the patient.
Oral manifestations of systematic disease are signs and symptoms of disease occurring elsewhere in the body detected in the oral cavity and oral secretions. High blood sugar can be detected by sampling saliva. Saliva sampling may be a non-invasive way to detect changes in the gut microbiome and changes in systemic disease. Another example is tertiary syphilis, where changes to teeth can occur. Syphilis infection can be associated with longitudinal furrows of the tongue.
Laser gingivectomy is a dental procedure that recontours or scalpels the gingival tissue to improve long term dental health or aesthetics. Compared to conventional scalpel surgery, soft-tissue dental lasers, such as Laser diode, Nd:YAG laser, Er:YAG laser, Er,Cr:YSGG laser, and CO2 lasers, can perform this procedure, offering a precise, stable, bloodless, often less painful, and accelerated healing experience. However, the Laser diode gained more popularity due to its versatility, less interaction with hard tissue, ease of use, and the less expensive set up.

Enamel-Renal syndrome is a rare autosomal recessive condition. This condition is also known as idiopathic multicentric osteolysis with nephropathy. It is characterised by dental abnormalities and nephrocalcinosis.