A mouth ulcer (aphtha) is an ulcer that occurs on the mucous membrane of the oral cavity. Mouth ulcers are very common, occurring in association with many diseases and by many different mechanisms, but usually there is no serious underlying cause. Rarely, a mouth ulcer that does not heal may be a sign of oral cancer. These ulcers may form individually or multiple ulcers may appear at once. Once formed, an ulcer may be maintained by inflammation and/or secondary infection.

Oral candidiasis, also known as oral thrush among other names, is candidiasis that occurs in the mouth. That is, oral candidiasis is a mycosis of Candida species on the mucous membranes of the mouth.

Oral leukoplakia is a potentially malignant disorder affecting the oral mucosa. It is defined as “essentially an oral mucosal white lesion that cannot be considered as any other definable lesion.” Oral leukoplakia is a white patch or plaque that develops in the oral cavity and is strongly associated with smoking.Leukoplakia is a firmly attached white patch on a mucous membrane which is associated with increased risk of cancer. The edges of the lesion are typically abrupt and the lesion changes with time. Advanced forms may develop red patches. There are generally no other symptoms. It usually occurs within the mouth, although sometimes mucosa in other parts of the gastrointestinal tract, urinary tract, or genitals may be affected.

Lichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Erythroplakia is a clinical term to describe any erythematous (red) area on a mucous membrane, that cannot be attributed to any other pathology.

Aphthous stomatitis, or recurrent aphthous stomatitis (RAS), is a common condition characterized by the repeated formation of benign and non-contagious mouth ulcers (aphthae) in otherwise healthy individuals. The informal term canker sore is also used, mainly in North America, although it may also refer to other types of mouth ulcers. The cause is not completely understood but involves a T cell-mediated immune response triggered by a variety of factors which may include nutritional deficiencies, local trauma, stress, hormonal influences, allergies, genetic predisposition, certain foods, dehydration, or some food additives.
A precancerous condition is a condition, tumor or lesion involving abnormal cells which are associated with an increased risk of developing into cancer. Clinically, precancerous conditions encompass a variety of abnormal tissues with an increased risk of developing into cancer. Some of the most common precancerous conditions include certain colon polyps, which can progress into colon cancer, monoclonal gammopathy of undetermined significance, which can progress into multiple myeloma or myelodysplastic syndrome. and cervical dysplasia, which can progress into cervical cancer. Bronchial premalignant lesions can progress to squamous cell carcinoma of the lung.

Stomatitis is inflammation of the mouth and lips. It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.
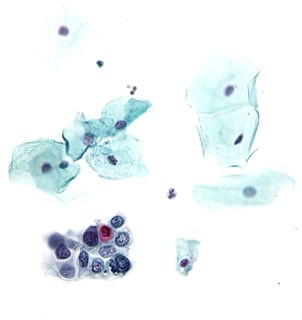
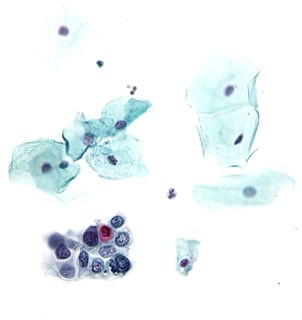
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which can reveal systemic conditions, such as diabetes or vitamin deficiency, or the local effects of chronic tobacco or alcohol use. The oral mucosa tends to heal faster and with less scar formation compared to the skin. The underlying mechanism remains unknown, but research suggests that extracellular vesicles might be involved.

Geographic tongue, also known by several other terms, is a condition of the mucous membrane of the tongue, usually on the dorsal surface. It is a common condition, affecting approximately 2–3% of the general population. It is characterized by areas of smooth, red depapillation which migrate over time. The name comes from the map-like appearance of the tongue, with the patches resembling the islands of an archipelago. The cause is unknown, but the condition is entirely benign, and there is no curative treatment. Uncommonly, geographic tongue may cause a burning sensation on the tongue, for which various treatments have been described with little formal evidence of efficacy.
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, measuring about 2mm or less. The lesion almost exclusively involves the hard palate, and in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and color of the mucosa may vary from pink to red.
An oral medicine or stomatology doctor has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region, essentially as a "physician of the mouth."

Necrotizing sialometaplasia (NS) is a benign, ulcerative lesion, usually located towards the back of the hard palate. It is thought to be caused by ischemic necrosis of minor salivary glands in response to trauma. Often painless, the condition is self-limiting and should heal in 6–10 weeks.
Leukoedema is a blue, grey or white appearance of mucosae, particularly the buccal mucosa ; it may also occur on the mucosa of the larynx or vagina. It is a harmless and very common condition. Because it is so common, it has been argued that it may in fact represent a variation of the normal appearance rather than a disease, but empirical evidence suggests that leukoedema is an acquired condition caused by local irritation. It is found more commonly in black skinned people and tobacco users. The term is derived from the Greek words λευκός leukós, "white" and οἴδημα oídēma, "swelling".

Smoker's melanosis is seen with the naked eye as a brown to black pigmentation of the oral tissue i.e. the gums, cheeks or palate as well as in larynx. It is most often seen in the lower labial gingiva of tobacco users. Most easily it is found in Caucasians, due to their lack of a genetically caused melanin pigmentation.
Oral and maxillofacial pathology refers to the diseases of the mouth, jaws and related structures such as salivary glands, temporomandibular joints, facial muscles and perioral skin. The mouth is an important organ with many different functions. It is also prone to a variety of medical and dental disorders.

Median rhomboid glossitis is a condition characterized by an area of redness and loss of lingual papillae on the central dorsum of the tongue, sometimes including lesions of the tongue and palate. It is seen in patients using inhaled steroids and smokers, and is usually a kind of chronic atrophic oral candidiasis, but hematinic deficiency and diabetes should be excluded.
Morsicatio buccarum is a condition characterized by chronic irritation or injury to the buccal mucosa, caused by repetitive chewing, biting or nibbling.
Denture-related stomatitis is a common condition where mild inflammation and redness of the oral mucous membrane occurs beneath a denture. In about 90% of cases, Candida species are involved, which are normally a harmless component of the oral microbiota in many people. Denture-related stomatitis is the most common form of oral candidiasis. It is more common in elderly people, and in those who wear a complete upper denture. Denture-related stomatitis is more likely to develop when the denture is left constantly in the mouth, rather than removing it during sleep, and when the denture is not cleaned regularly.
Smokeless tobacco keratosis (STK) is a condition which develops on the oral mucosa in response to smokeless tobacco use. Generally it appears as a white patch, located at the point where the tobacco is held in the mouth. The condition usually disappears once the tobacco habit is stopped. It is associated with slightly increased risk of mouth cancer.