Related Research Articles

Mumps is a viral disease caused by the mumps virus. Initial symptoms are non-specific and include fever, headache, malaise, muscle pain, and loss of appetite. These symptoms are usually followed by painful swelling of the parotid glands, called parotitis, which is the most common symptom of infection. Symptoms typically occur 16 to 18 days after exposure to the virus and resolve within two weeks. About one third of infections are asymptomatic.

The salivary glands in mammals are exocrine glands that produce saliva through a system of ducts. Humans have three paired major salivary glands, as well as hundreds of minor salivary glands. Salivary glands can be classified as serous, mucous, or seromucous (mixed).

The great auricular nerve is a cutaneous nerve of the head. It originates from the cervical plexus, with branches of spinal nerves C2 and C3. It provides sensory innervation to the skin over the parotid gland and the mastoid process of the temporal bone, and surfaces of the outer ear.

The parotid gland is a major salivary gland in many animals. In humans, the two parotid glands are present on either side of the mouth and in front of both ears. They are the largest of the salivary glands. Each parotid is wrapped around the mandibular ramus, and secretes serous saliva through the parotid duct into the mouth, to facilitate mastication and swallowing and to begin the digestion of starches. There are also two other types of salivary glands; they are submandibular and sublingual glands. Sometimes accessory parotid glands are found close to the main parotid glands.

Parotitis is an inflammation of one or both parotid glands, the major salivary glands located on either side of the face, in humans. The parotid gland is the salivary gland most commonly affected by inflammation.

Ear pain, also known as earache or otalgia, is pain in the ear. Primary ear pain is pain that originates from the ear. Secondary ear pain is a type of referred pain, meaning that the source of the pain differs from the location where the pain is felt.
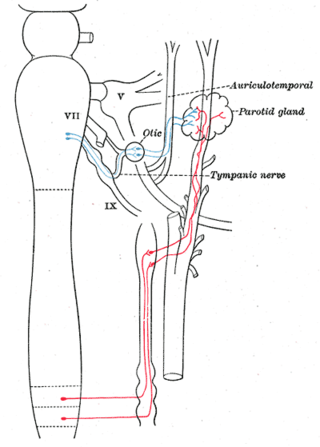
The auriculotemporal nerve is a branch of the mandibular nerve (CN V3) that runs with the superficial temporal artery and vein, and provides sensory innervation to various regions on the side of the head.
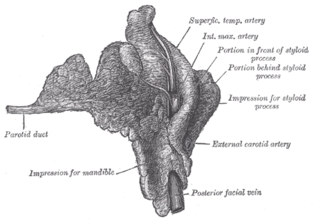
The parotid duct, or Stensen duct, is a salivary duct. It is the route that saliva takes from the major salivary gland, the parotid gland, into the mouth. It opens into the mouth opposite the second upper molar tooth.

Pleomorphic adenoma is a common benign salivary gland neoplasm characterised by neoplastic proliferation of epithelial (ductal) cells along with myoepithelial components, having a malignant potentiality. It is the most common type of salivary gland tumor and the most common tumor of the parotid gland. It derives its name from the architectural Pleomorphism seen by light microscopy. It is also known as "Mixed tumor, salivary gland type", which refers to its dual origin from epithelial and myoepithelial elements as opposed to its pleomorphic appearance.

Sialadenitis (sialoadenitis) is inflammation of salivary glands, usually the major ones, the most common being the parotid gland, followed by submandibular and sublingual glands. It should not be confused with sialadenosis (sialosis) which is a non-inflammatory enlargement of the major salivary glands.

Sialolithiasis is a crystallopathy where a calcified mass or sialolith forms within a salivary gland, usually in the duct of the submandibular gland. Less commonly the parotid gland or rarely the sublingual gland or a minor salivary gland may develop salivary stones.
Uveoparotitis is a symptom of sarcoidosis. It describes a chronic inflammation of the parotid gland (parotitis) and part of the eye called the uvea (uveitis). There is also a phenomenon called Waldenström's uveoparotitis, where the symptom is related to Heerfordt's syndrome. The condition was first described in 1909.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Heerfordt syndrome is a rare manifestation of sarcoidosis. The symptoms include inflammation of the eye (uveitis), swelling of the parotid gland, chronic fever, and in some cases, palsy of the facial nerves.

Otitis externa, also called swimmer's ear, is inflammation of the ear canal. It often presents with ear pain, swelling of the ear canal, and occasionally decreased hearing. Typically there is pain with movement of the outer ear. A high fever is typically not present except in severe cases.

Salivary gland diseases (SGDs) are multiple and varied in cause. There are three paired major salivary glands in humans – the parotid glands, the submandibular glands, and the sublingual glands. In addition there are about 800-1000 minor salivary glands in the mucosa of the mouth. The parotid gland is located in front of each ear, and secretes mostly serous saliva via the parotid duct into the mouth, usually opening roughly opposite the maxillary second molar. The submandibular gland is located medial to the angle of the mandible, and it drains its mixture of serous and mucous saliva via the submandibular duct into the mouth, usually opening in a punctum located in the floor of mouth. The sublingual gland is located below the tongue, on the floor of the mouth. It drains its mostly mucous saliva into the mouth via about 8-20 ducts which open along the plica sublingualis.
A sialocele is a localized, subcutaneous cavity containing saliva. It is caused by trauma or infection. They most commonly develop about 8–14 days after injury.

A parotidectomy is the surgical excision (removal) of the parotid gland, the major and largest of the salivary glands. The procedure is most typically performed due to neoplasms (tumors), which are growths of rapidly and abnormally dividing cells. Neoplasms can be benign (non-cancerous) or malignant (cancerous). The majority of parotid gland tumors are benign, however 20% of parotid tumors are found to be malignant. Parotidectomy is performed mostly by oral and maxillofacial surgeon and ENT surgeon.

Pneumatosis is the abnormal presence of air or other gas within tissues.
A cervical thymic cyst, also called thymopharyngeal duct cyst, is a fluid-filled mass that occurs when the thymopharyngeal duct, an embryonic structure connecting the nascent thymus with the embryonic pharynx, fails to close and disappear. A thymic cyst is typically a solitary mass on one side of the neck, and is usually found near the carotid sheath. Some cervical thymic cysts may extend into the mediastinum. It is usually asymptomatic. The diagnostic process includes differentiating between other causes of neck masses in infants and children, including branchial cleft cysts and cystic hygromas. The treatment is surgical excision. On histologic examination, the wall of the cyst includes thymic tissue, and may include parathyroid gland tissue because of the parathyroid gland's common embryonic origin with the thymus gland in the third pharyngeal pouch. Fewer than 100 cases of cervical thymic cysts have been reported in the medical literature.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Joiner MC; van der Kogel A (15 June 2016). Basic Clinical Radiobiology, Fifth Edition. CRC Press. p. 1908. ISBN 978-0-340-80893-1.
- 1 2 3 Gibson AM; Benko KR (5 May 2013). Head, Eyes, Ears, Nose, and Throat Emergencies, An Issue of Emergency Medicine Clinics. Elsevier Health Sciences. p. 124. ISBN 978-1-4557-7171-4.
- ↑ McCormick, Michael E.; Bawa, Gurneet; Shah, Rahul K. (2013). "Idiopathic recurrent pneumoparotitis". American Journal of Otolaryngology. 34 (2): 180–182. doi:10.1016/j.amjoto.2012.11.005. ISSN 0196-0709. PMID 23318047.
- 1 2 Mukherji SK; Chong V (1 January 2011). Atlas of Head and Neck Imaging: The Extracranial Head and Neck. Thieme. p. 147. ISBN 978-1-60406-525-1.
- 1 2 3 4 Goguen, LA; April, MM; Karmody, CS; Carter, BL (December 1995). "Self-induced pneumoparotitis". Archives of Otolaryngology–Head & Neck Surgery. 121 (12): 1426–9. doi:10.1001/archotol.1995.01890120082017. PMID 7488376.
- ↑ Kreuter, M; Kreuter, C; Herth, F (February 2008). "[Pneumological aspects of wind instrument performance--physiological, pathophysiological and therapeutic considerations]". Pneumologie (Stuttgart, Germany). 62 (2): 83–7. doi:10.1055/s-2007-996164. PMID 18075966.
- 1 2 Ferlito, A; Andretta, M; Baldan, M; Candiani, F (June 1992). "Non-occupational recurrent bilateral pneumoparotitis in an adolescent". The Journal of Laryngology and Otology. 106 (6): 558–60. doi:10.1017/s0022215100120146. PMID 1624898.
- ↑ Markowitz-Spence, L; Brodsky, L; Seidell, G; Stanievich, JF (December 1987). "Self-induced pneumoparotitis in an adolescent. Report of a case and review of the literature". International Journal of Pediatric Otorhinolaryngology. 14 (2–3): 113–21. doi:10.1016/0165-5876(87)90021-8. PMID 3325441.