Radiography is an imaging technique using X-rays, gamma rays, or similar ionizing radiation and non-ionizing radiation to view the internal form of an object. Applications of radiography include medical and industrial radiography. Similar techniques are used in airport security,. To create an image in conventional radiography, a beam of X-rays is produced by an X-ray generator and it is projected towards the object. A certain amount of the X-rays or other radiation are absorbed by the object, dependent on the object's density and structural composition. The X-rays that pass through the object are captured behind the object by a detector. The generation of flat two-dimensional images by this technique is called projectional radiography. In computed tomography, an X-ray source and its associated detectors rotate around the subject, which itself moves through the conical X-ray beam produced. Any given point within the subject is crossed from many directions by many different beams at different times. Information regarding the attenuation of these beams is collated and subjected to computation to generate two-dimensional images on three planes which can be further processed to produce a three-dimensional image.

Radiology is the medical discipline that uses medical imaging to diagnose diseases and guide their treatment, within the bodies of humans and other animals. It began with radiography, but today it includes all imaging modalities, including those that use no electromagnetic radiation, as well as others that do, such as computed tomography (CT), fluoroscopy, and nuclear medicine including positron emission tomography (PET). Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.

Mammography is the process of using low-energy X-rays to examine the human breast for diagnosis and screening. The goal of mammography is the early detection of breast cancer, typically through detection of characteristic masses or microcalcifications.

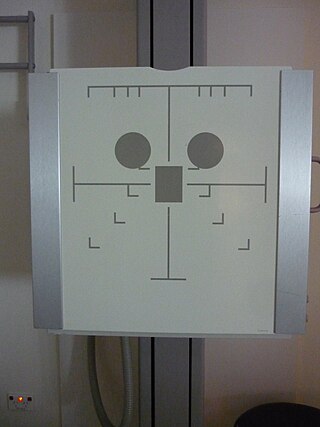
An X-ray machine is a device that uses X-rays for a variety of applications including medicine, X-ray fluorescence, electronic assembly inspection, and measurement of material thickness in manufacturing operations. In medical applications, X-ray machines are used by radiographers to acquire x-ray images of the internal structures of living organisms, and also in sterilization.

Fluoroscopy is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope allows a surgeon to see the internal structure and function of a patient, so that the pumping action of the heart or the motion of swallowing, for example, can be watched. This is useful for both diagnosis and therapy and occurs in general radiology, interventional radiology, and image-guided surgery.

Caesium iodide or cesium iodide is the ionic compound of caesium and iodine. It is often used as the input phosphor of an X-ray image intensifier tube found in fluoroscopy equipment. Caesium iodide photocathodes are highly efficient at extreme ultraviolet wavelengths.
An X-ray image intensifier (XRII) is an image intensifier that converts X-rays into visible light at higher intensity than the more traditional fluorescent screens can. Such intensifiers are used in X-ray imaging systems to allow low-intensity X-rays to be converted to a conveniently bright visible light output. The device contains a low absorbency/scatter input window, typically aluminum, input fluorescent screen, photocathode, electron optics, output fluorescent screen and output window. These parts are all mounted in a high vacuum environment within glass or, more recently, metal/ceramic. By its intensifying effect, It allows the viewer to more easily see the structure of the object being imaged than fluorescent screens alone, whose images are dim. The XRII requires lower absorbed doses due to more efficient conversion of X-ray quanta to visible light. This device was originally introduced in 1948.
Digital radiography is a form of radiography that uses x-ray–sensitive plates to directly capture data during the patient examination, immediately transferring it to a computer system without the use of an intermediate cassette. Advantages include time efficiency through bypassing chemical processing and the ability to digitally transfer and enhance images. Also, less radiation can be used to produce an image of similar contrast to conventional radiography.

Projectional radiography, also known as conventional radiography, is a form of radiography and medical imaging that produces two-dimensional images by X-ray radiation. The image acquisition is generally performed by radiographers, and the images are often examined by radiologists. Both the procedure and any resultant images are often simply called 'X-ray'. Plain radiography or roentgenography generally refers to projectional radiography. Plain radiography can also refer to radiography without a radiocontrast agent or radiography that generates single static images, as contrasted to fluoroscopy, which are technically also projectional.

Tomosynthesis, also digital tomosynthesis (DTS), is a method for performing high-resolution limited-angle tomography at radiation dose levels comparable with projectional radiography. It has been studied for a variety of clinical applications, including vascular imaging, dental imaging, orthopedic imaging, mammographic imaging, musculoskeletal imaging, and chest imaging.
Photostimulated luminescence (PSL) is the release of stored energy within a phosphor by stimulation with visible light, to produce a luminescent signal. X-rays may induce such an energy storage. A plate based on this mechanism is called a photostimulable phosphor (PSP) plate and is one type of X-ray detector used in projectional radiography. Creating an image requires illuminating the plate twice: the first exposure, to the radiation of interest, "writes" the image, and a later, second illumination "reads" the image. The device to read such a plate is known as a phosphorimager.
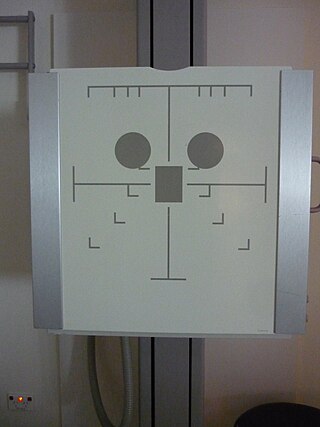
Automatic Exposure Control (AEC) is an X-ray exposure termination device. A medical radiographic exposure is always initiated by a human operator but an AEC detector system may be used to terminate the exposure when a predetermined amount of radiation has been received. The intention of AEC is to provide consistent x-ray image exposure, whether to film, a digital detector or a CT scanner. AEC systems may also automatically set exposure factors such as the X-ray tube current and voltage in a CT.

Neutron imaging is the process of making an image with neutrons. The resulting image is based on the neutron attenuation properties of the imaged object. The resulting images have much in common with industrial X-ray images, but since the image is based on neutron attenuating properties instead of X-ray attenuation properties, some things easily visible with neutron imaging may be very challenging or impossible to see with X-ray imaging techniques.

X-ray detectors are devices used to measure the flux, spatial distribution, spectrum, and/or other properties of X-rays.

Photon counting is a technique in which individual photons are counted using a single-photon detector (SPD). A single-photon detector emits a pulse of signal for each detected photon. The counting efficiency is determined by the quantum efficiency and the system's electronic losses.

Amorphous silicon (a-Si) is the non-crystalline form of silicon used for solar cells and thin-film transistors in LCDs.
Jeffrey Harold Siewerdsen is an American physicist and biomedical engineer who is a Professor of Imaging Physics at The University of Texas MD Anderson Cancer Center as well as Biomedical Engineering, Computer Science, Radiology, and Neurosurgery at Johns Hopkins University.He is among the original inventors of cone-beam CT-guided radiotherapy as well as weight-bearing cone-beam CT for musculoskeletal radiology and orthopedic surgery. His work also includes the early development of flat-panel detectors on mobile C-arms for intraoperative cone-beam CT in image-guided surgery. He developed early models for the signal and noise performance of flat-panel detectors and later extended such analysis to dual-energy imaging and 3D imaging performance in cone-beam CT. He founded the ISTAR Lab in the Department of Biomedical Engineering, the Carnegie Center for Surgical Innovation at Johns Hopkins Hospital, and the Surgical Data Science Program at the Institute for Data Science in Oncology at The University of Texas MD Anderson Cancer Center.
Photon-counting computed tomography (PCCT) is a form of X-ray computed tomography (CT) in which X-rays are detected using a photon-counting detector (PCD) which registers the interactions of individual photons. By keeping track of the deposited energy in each interaction, the detector pixels of a PCD each record an approximate energy spectrum, making it a spectral or energy-resolved CT technique. In contrast, more conventional CT scanners use energy-integrating detectors (EIDs), where the total energy deposited in a pixel during a fixed period of time is registered. These EIDs thus register only photon intensity, comparable to black-and-white photography, whereas PCDs register also spectral information, similar to color photography.
Spectral imaging is an umbrella term for energy-resolved X-ray imaging in medicine. The technique makes use of the energy dependence of X-ray attenuation to either increase the contrast-to-noise ratio, or to provide quantitative image data and reduce image artefacts by so-called material decomposition. Dual-energy imaging, i.e. imaging at two energy levels, is a special case of spectral imaging and is still the most widely used terminology, but the terms "spectral imaging" and "spectral CT" have been coined to acknowledge the fact that photon-counting detectors have the potential for measurements at a larger number of energy levels.
Photon-counting mammography was introduced commercially in 2003 and was the first widely available application of photon-counting detector technology in medical x-ray imaging. Photon-counting mammography improves dose efficiency compared to conventional technologies, and enables spectral imaging.