Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid use disorder. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Withdrawal management using methadone can be accomplished in less than a month, or it may be done gradually over a longer period of time, or simply maintained for the rest of the patient's life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.

Harm reduction, or harm minimization, refers to a range of intentional practices and public health policies designed to lessen the negative social and/or physical consequences associated with various human behaviors, both legal and illegal. Harm reduction is used to decrease negative consequences of recreational drug use and sexual activity without requiring abstinence, recognizing that those unable or unwilling to stop can still make positive change to protect themselves and others.

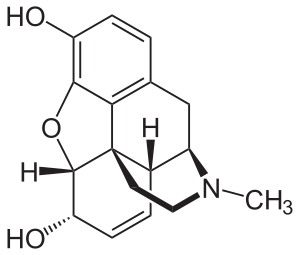
Naloxone is an opioid antagonist: a medication used to reverse or reduce the effects of opioids. For example, it is used to restore breathing after an opioid overdose. Effects begin within two minutes when given intravenously, five minutes when injected into a muscle, and ten minutes as a nasal spray. Naloxone blocks the effects of opioids for 30 to 90 minutes.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, the patient must have moderate opioid withdrawal symptoms before buprenorphine can be administered under direct observation of a health-care provider.

Naltrexone, sold under the brand name Revia among others, is a medication primarily used to manage alcohol use or opioid use disorder by reducing cravings and feelings of euphoria associated with substance use disorder. It has also been found effective in the treatment of other addictions and may be used for them off-label. An opioid-dependent person should not receive naltrexone before detoxification. It is taken by mouth or by injection into a muscle. Effects begin within 30 minutes, though a decreased desire for opioids may take a few weeks to occur. Side effects may include trouble sleeping, anxiety, nausea, and headaches. In those still on opioids, opioid withdrawal may occur. Use is not recommended in people with liver failure. It is unclear if use is safe during pregnancy. Naltrexone is an opioid antagonist and works by blocking the effects of opioids, including both opioid drugs as well as opioids naturally produced in the brain.
Substance dependence, also known as drug dependence, is a biopsychological situation whereby an individual's functionality is dependent on the necessitated re-consumption of a psychoactive substance because of an adaptive state that has developed within the individual from psychoactive substance consumption that results in the experience of withdrawal and that necessitates the re-consumption of the drug. A drug addiction, a distinct concept from substance dependence, is defined as compulsive, out-of-control drug use, despite negative consequences. An addictive drug is a drug which is both rewarding and reinforcing. ΔFosB, a gene transcription factor, is now known to be a critical component and common factor in the development of virtually all forms of behavioral and drug addictions, but not dependence.
A methadone clinic is a medical facility where medications for opioid use disorder (MOUD) are dispensed-—historically and most commonly methadone, although buprenorphine is also increasingly prescribed. Medically assisted drug therapy treatment is indicated in patients who are opioid-dependent or have a history of opioid dependence. Methadone is a schedule II (USA) opioid analgesic, that is also prescribed for pain management. It is a long-acting opioid that can delay the opioid withdrawal symptoms that patients experience from taking short-acting opioids, like heroin, and allow time for withdrawal management. In the United States, by law, patients must receive methadone under the supervision of a physician, and dispensed through an Opioid Treatment Program (OTP) certified by the Substance Abuse and Mental Health Services Administration and registered with the Drug Enforcement Administration.

An opioid antagonist, or opioid receptor antagonist, is a receptor antagonist that acts on one or more of the opioid receptors.
Drug detoxification is variously construed or interpreted as a type of "medical" intervention or technique in regards to a physical dependence mediated by a drug; as well as the process and experience of a withdrawal syndrome or any of the treatments for acute drug overdose (toxidrome). The first definition however, in relation to substance dependence and its treatment is arguably a misnomer and even directly contradictory since withdrawal is neither contingent upon nor alleviated through biological excretion or clearance of the drug. In fact, excretion of a given drug from the body is one of the very processes that leads to withdrawal since the syndrome arises largely due to the cessation itself and the drug being absent from the body; especially the blood plasma, not from ‘leftover toxins’ or traces of the drug still being in the system.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia from slow and shallow breathing. Other symptoms include small pupils and unconsciousness; however, its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.

Substance use disorder (SUD) is the persistent use of drugs despite the substantial harm and adverse consequences to one's own self and others, as a result of their use. In perspective, the effects of the wrong use of substances that are capable of causing harm to the user or others, have been extensively described in different studies using a variety of terms such as substance use problems, problematic drugs or alcohol use, and substance use disorder. The National Institute of Mental Health (NIMH) states that "Substance use disorder (SUD) is a treatable mental disorder that affects a person's brain and behavior, leading to their inability to control their use of substances like legal or illegal drugs, alcohol, or medications. Symptoms can be moderate to severe, with addiction being the most severe form of SUD". Substance use disorders (SUD) are considered to be a serious mental illness that fluctuates with the age that symptoms first start appearing in an individual, the time during which it exists and the type of substance that is used. It is not uncommon for those who have SUD to also have other mental health disorders. Substance use disorders are characterized by an array of mental/emotional, physical, and behavioral problems such as chronic guilt; an inability to reduce or stop consuming the substance(s) despite repeated attempts; operating vehicles while intoxicated; and physiological withdrawal symptoms. Drug classes that are commonly involved in SUD include: alcohol (alcoholism); cannabis; opioids; stimulants such as nicotine, cocaine and amphetamines; benzodiazepines; barbiturates; and other substances.
Neonatal withdrawal or neonatal abstinence syndrome (NAS) or neonatal opioid withdrawal syndrome (NOWS) is a withdrawal syndrome of infants after birth caused by in utero exposure to drugs of dependence, most commonly opioids. Common signs and symptoms include tremors, irritability, vomiting, diarrhea, and fever. NAS is primarily diagnosed with a detailed medication history and scoring systems. First-line treatment should begin with non-medication interventions to support neonate growth, though medication interventions may be used in certain situations.

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek.

There is an ongoing opioid epidemic in the United States, originating out of both medical prescriptions and illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management, resulting in a rise in overall opioid use throughout subsequent years.

The opioid epidemic, also referred to as the opioid crisis, is the rapid increase in the overuse, misuse/abuse, and overdose deaths attributed either in part or in whole to the class of drugs called opiates/opioids since the 1990s. It includes the significant medical, social, psychological, demographic and economic consequences of the medical, non-medical, and recreational abuse of these medications.
Clinical Opiate Withdrawal Scale (COWS) is a method used by registered practitioners to measure the severity of a patient's opioid withdrawal symptoms. This method consists of a series of 11 topics each comprising 4 - 5 common symptoms experienced by a patient undergoing opioid withdrawal. In each topic a rank is given depending on what the patient responds to. Generally, 0 is considered to be no symptom shown and 4 or 5 is considered to be the most common and severe symptom shown. These results are then added up and a final diagnosis is made based on the value obtained. This test is crucial as it allows the practitioner to assess the physiological and psychological behaviours of the patient as well as the severity of each symptom during the duration of the examination. The results are grouped into 3 categories of mild, moderately severe and severe. Mild consists of 5 to 12 points, moderately severe consists of 13 to 24 points and anything above 36 points is severe and requires direct medical attention.

Opioid withdrawal is a set of symptoms arising from the sudden withdrawal or reduction of opioids where previous usage has been heavy and prolonged. Signs and symptoms of withdrawal can include drug craving, anxiety, restless legs, nausea, vomiting, diarrhea, sweating, and an increased heart rate. Opioid use triggers a rapid adaptation in cellular signalling pathways that means, when rapidly withdrawn, there can be adverse physiological effects. All opioids, both recreational drugs and medications, when reduced or stopped, can lead to opioid withdrawal symptoms. When withdrawal symptoms are due to recreational opioid use, the term opioid use disorder is used, whereas when due to prescribed medications, the term prescription opioid use disorder is used. Opioid withdrawal can be helped by the use of opioid replacement therapy, and symptoms may be relieved by the use of medications including lofexidine and clonidine.
Opioid agonist therapy (OAT) is a treatment in which prescribed opioid agonists are given to patients who live with Opioid use disorder (OUD). In the case of methadone maintenance treatment (MMT), methadone is used to treat dependence on heroin or other opioids, and is administered on an ongoing basis.

Prescription drug addiction is the chronic, repeated use of a prescription drug in ways other than prescribed for, including using someone else’s prescription. A prescription drug is a pharmaceutical drug that may not be dispensed without a legal medical prescription. Drugs in this category are supervised due to their potential for misuse and substance use disorder. The classes of medications most commonly abused are opioids, central nervous system (CNS) depressants and central nervous stimulants. In particular, prescription opioid is most commonly abused in the form of prescription analgesics.
Harm reduction consists of a series of strategies aimed at reducing the negative impacts of drug use on users. It has been described as an alternative to the U.S.'s moral model and disease model of drug use and addiction. While the moral model treats drug use as a morally wrong action and the disease model treats it as a biological or genetic disease needing medical intervention, harm reduction takes a public health approach with a basis in pragmatism. Harm reduction provides an alternative to complete abstinence as a method for preventing and mitigating the negative consequences of drug use and addiction.