Vaccination is the administration of a vaccine to help the immune system develop protection from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them. The effectiveness of vaccination has been widely studied and verified. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. However, some diseases, such as measles outbreaks in America, have seen rising cases due to relatively low vaccination rates in the 2010s - attributed, in part, to vaccine hesitancy.

Measles is a highly contagious infectious disease caused by measles virus. Symptoms usually develop 10–12 days after exposure to an infected person and last 7–10 days. Initial symptoms typically include fever, often greater than 40 °C (104 °F), cough, runny nose, and inflamed eyes. Small white spots known as Koplik's spots may form inside the mouth two or three days after the start of symptoms. A red, flat rash which usually starts on the face and then spreads to the rest of the body typically begins three to five days after the start of symptoms. Common complications include diarrhea, middle ear infection (7%), and pneumonia (6%). These occur in part due to measles-induced immunosuppression. Less commonly seizures, blindness, or inflammation of the brain may occur. Other names include morbilli, rubeola, red measles, and English measles. Both rubella, also known as German measles, and roseola are different diseases caused by unrelated viruses.
Vaccine hesitancy, also known as anti-vaccination or anti-vax, is a reluctance or refusal to be vaccinated or to have one's children vaccinated against contagious diseases. People who subscribe to this view are commonly known as "anti-vaxxers". The term encompasses outright refusal to vaccinate, delaying vaccines, accepting vaccines but remaining uncertain about their use, or using certain vaccines but not others. Arguments against vaccination are contradicted by overwhelming scientific consensus about the safety and efficacy of vaccines. The World Health Organization views vaccine hesitancy as one of the top ten global health threats.
The Expanded Program on Immunization(EPI) in the Philippines began in July 1979. And, in 1986, made a response to the Universal Child Immunization goal. The four major strategies include:
- sustaining high routine Full Immunized Child (FIC) coverage of at least 90% in all provinces and cities;
- sustaining the polio-free country for global certification;
- eliminating measles by 2008; and
- eliminating neonatal tetanus by 2008.
Vaccination policy is the health policy a government adopts in relation to vaccination. Vaccination policies have been developed over the approximately two centuries since the invention of vaccination with the purpose of eradicating disease from, or creating a herd immunity for, the population the government aims to protect. Vaccination advisory committees within each country are usually responsible for providing information to governments that is used to make evidence-based decisions regarding vaccine and immunization policy.

Eradication is the reduction of an infectious disease's prevalence in the global host population to zero. It is sometimes confused with elimination, which describes either the reduction of an infectious disease's prevalence in a regional population to zero or the reduction of the global prevalence to a negligible amount. Further confusion arises from the use of the term eradication to refer to the total removal of a given pathogen from an individual, particularly in the context of HIV and certain other viruses where such cures are sought.
Health in the United States is the overall health of the population of the United States. Many diseases, including COVID-19, have spread rapidly throughout the country. Notable pandemics have also struck, including the Influenza pandemic of 1918. Recently, obesity has also become a struggle for the United States population.

Measles vaccine protects against becoming infected with measles. Nearly all of those who do not develop immunity after a single dose develop it after a second dose. When rates of vaccination within a population are greater than 92%, outbreaks of measles typically no longer occur; however, they may occur again if rates of vaccination decrease. The vaccine's effectiveness lasts many years. It is unclear if it becomes less effective over time. The vaccine may also protect against measles if given within a couple of days after exposure to measles.
Dengue vaccine is a vaccine used to prevent dengue fever in humans. As of 2019, one version is commercially available, known as CYD-TDV, and sold under the brand name Dengvaxia. The vaccine is only recommended in those who have previously had dengue fever or populations in which most people have been previously infected. The value of the vaccine is limited by the fact that it may increase the risk of severe dengue in those who have not previously been infected. It is given as three injections over a year.

Measles is extremely contagious, but surviving the infection results in lifelong immunity, so its continued circulation in a community depends on the generation of susceptible hosts by birth of children. In communities which generate insufficient new hosts the disease will die out. This concept was first recognized by Bartlett in 1957, who referred to the minimum number supporting measles as the critical community size (CCS). Analysis of outbreaks in island communities suggested that the CCS for measles is c. 250,000.
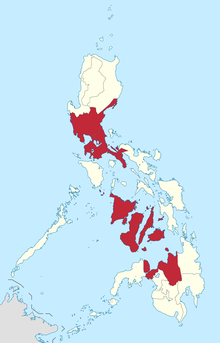
The Dengvaxia controversy was a health scare in the Philippines caused when the dengue fever vaccine Dengvaxia was found to increase the risk of disease severity for some people who had received it. A vaccination program had been run by the Philippine Department of Health (DOH) who had administered Sanofi Pasteur's Dengvaxia to schoolchildren.
In early 2019, a measles outbreak occurred in the Portland metropolitan area, including the Clark County, Washington suburbs, in the United States. At the time, the outbreak was the largest outbreak in more than two decades; outbreaks in 2019 in areas including Brooklyn and Rockland County, New York have since seen far greater numbers of cases.
The 2019 measles outbreaks refer to a substantial global increase in the number of measles cases reported, relative to 2018. As of April 2019, the number of measles cases reported worldwide represented a 300% increase from the number of cases seen in the previous year, constituting over 110,000 measles cases reported in the first three months of 2019. In the first half of 2019, the World Health Organization received reports of 364,808 measles cases from 182 countries, up 182% from the same time period of 2018 when 129,239 confirmed cases were reported by 181 countries.

Measles was declared eliminated from the United States in 2000 by the World Health Organization due to the success of vaccination efforts. However, it continues to be reintroduced by international travelers, and in recent years, anti-vaccination sentiment has allowed for the reemergence of measles outbreaks.
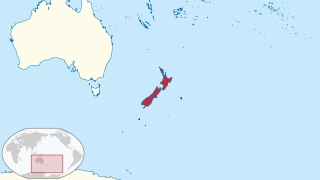
The 2019–2020 New Zealand measles outbreak was an epidemic that affected New Zealand, primarily the Auckland region. The outbreak was the worst epidemic in New Zealand since an influenza epidemic in 1999, and is the worst measles epidemic since 1938.
The 2019–2020 Philippines polio outbreak is an ongoing epidemic. For the past 19 years, the Philippines was free of any polio-related diseases. It was until September 14, 2019, when the disease began to resurface through a positive test result done to a 3-year-old girl from Mindanao. After the confirmation of a second case from tests done on a 5-year-old boy, the government of the Philippines publicly declared the polio outbreak on September 19, 2019.

In 2019, a measles epidemic broke out in the Democratic Republic of the Congo (DRC). The epidemic started in early 2019 in the southeast corner of the DRC and then spread to all provinces. By June 2019 the epidemic was reported to have exceeded the death toll of the concurrent Ebola epidemic. By April 2020, it had infected more than 341,000 people and claimed about 6,400 fatalities. This has primarily affected children under the age of five, representing 74% of infections and nearly 90% of deaths.

The 2019 Samoa measles outbreak began in September 2019. As of 6 January 2020, there were over 5,700 cases of measles and 83 deaths, out of a Samoan population of 200,874. Over three percent of the population were infected. The cause of the outbreak was attributed to decreased vaccination rates, from 74% in 2017 to 31–34% in 2018, even though nearby islands had rates near 99%.

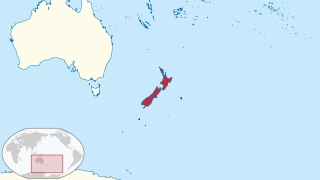
The 2019 Tonga measles outbreak began in October 2019 after a squad of Tongan rugby players came back from New Zealand. The epidemic as of December 8 is currently ongoing. As of January 5, there have been 612 cases of measles.

The COVID-19 vaccination program in the Philippines is an ongoing immunization campaign against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), in response to the ongoing pandemic in the country.