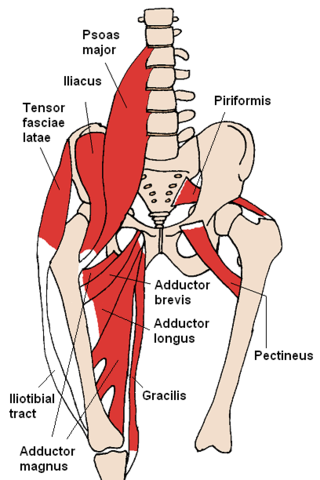
Iliotibial band syndrome (ITBS) is the second most common knee injury, and is caused by inflammation located on the lateral aspect of the knee due to friction between the iliotibial band and the lateral epicondyle of the femur. Pain is felt most commonly on the lateral aspect of the knee and is most intensive at 30 degrees of knee flexion. Risk factors in women include increased hip adduction and knee internal rotation. Risk factors seen in men are increased hip internal rotation and knee adduction. ITB syndrome is most associated with long-distance running, cycling, weight-lifting, and with military training.

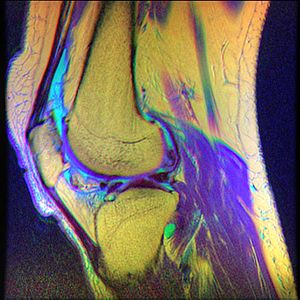
In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

The patella, also known as the kneecap, is a flat, rounded triangular bone which articulates with the femur and covers and protects the anterior articular surface of the knee joint. The patella is found in many tetrapods, such as mice, cats, birds and dogs, but not in whales, or most reptiles.

A luxating patella, sometimes called a trick knee, is a condition in which the patella, or kneecap, dislocates or moves out of its normal location. It can be associated with damage to the anterior cruciate ligament.

Osgood–Schlatter disease (OSD) is inflammation of the patellar ligament at the tibial tuberosity (apophysitis). It is characterized by a painful bump just below the knee that is worse with activity and better with rest. Episodes of pain typically last a few weeks to months. One or both knees may be affected and flares may recur.
Runner's knee may refer to a number of overuse injuries involving pain around the kneecap (patella), such as:

Patellar tendinitis, also known as jumper's knee, is an overuse injury of the tendon that straightens the knee. Symptoms include pain in the front of the knee. Typically the pain and tenderness is at the lower part of the kneecap, though the upper part may also be affected. Generally there is no pain when the person is at rest. Complications may include patellar tendon rupture.

Osteochondritis dissecans is a joint disorder primarily of the subchondral bone in which cracks form in the articular cartilage and the underlying subchondral bone. OCD usually causes pain during and after sports. In later stages of the disorder there will be swelling of the affected joint which catches and locks during movement. Physical examination in the early stages does only show pain as symptom, in later stages there could be an effusion, tenderness, and a crackling sound with joint movement.
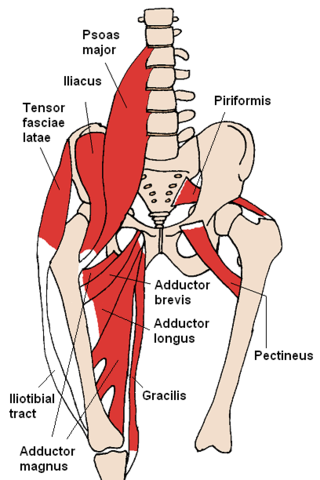
Snapping hip syndrome, also referred to as dancer's hip, is a medical condition characterized by a snapping sensation felt when the hip is flexed and extended. This may be accompanied by a snapping or popping noise and pain or discomfort. Pain often decreases with rest and diminished activity. Snapping hip syndrome is commonly classified by the location of the snapping as either extra-articular or intra-articular.
The knee examination, in medicine and physiotherapy, is performed as part of a physical examination, or when a patient presents with knee pain or a history that suggests a pathology of the knee joint.

Nail–patella syndrome is a genetic disorder that results in small, poorly developed nails and kneecaps, but can also affect many other areas of the body, such as the elbows, chest, and hips. The name "nail–patella" can be very misleading because the syndrome often affects many other areas of the body, including even the production of certain proteins. The severity of these effects varies depending on the individual. It is also referred to as iliac horn syndrome, hereditary onychoosteodysplasia, Fong disease or Turner–Kieser syndrome.
Plica syndrome is a condition that occurs when a plica becomes irritated, enlarged, or inflamed.

Patellofemoral pain syndrome is knee pain as a result of problems between the kneecap and the femur. The pain is generally in the front of the knee and comes on gradually. Pain may worsen with sitting, excessive use, or climbing and descending stairs.
A lateral release is a surgical procedure to release tight capsular structures on the outer aspect of the kneecap (patella). This is usually performed because of knee pain related to the kneecap being pulled over to the outer (lateral) side and not being able to run properly in the centre of the groove of the femur bone as the knee bends and straightens. The procedure is also known as a 'lateral retinacular release'.
Patellar subluxation syndrome, is an injury that is concerned with the kneecap. Patellar subluxation is more common than patellar dislocation and is just as disabling.

A patellar dislocation is a knee injury in which the patella (kneecap) slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place. Complications may include a patella fracture or arthritis.

Knee pain is pain in or around the knee.
Anterior interval release (AIR) is a type of arthroscopic knee surgery performed to alleviate pain and associated symptoms caused by scar tissue accumulation in the anterior region of the knee, behind and under the knee cap, in a condition called arthrofibrosis. In normal, asymptomatic knees, this anterior compartment of the knee comprises mobile, scar-free tissues such as the infrapatellar (Hoffa's) fat pad. With progression, scar tissue leads to closure of the anterior interval, tethering the patella tendon and causing pain, loss of range of motion, damage to knee cartilage, and/or pain, among other symptoms.

In medicine, Clarke's test is a component of knee examination which may be used to test for patellofemoral pain syndrome, chondromalacia patellae, patellofemoral arthritis, or anterior knee pain. It is not a standard part of the knee examination but is used to diagnose anterior knee pain where the history indicates this as the likely pathology. The patient is asked to actively contract the quadriceps muscle while the examiner's hand exerts pressure on the superior pole of the patella, so trying to prevent the proximal movement of the patella. While it can produce some discomfort even in normal people, the reproduction of the symptoms suggest pain of patellofemoral origin.
Running injuries affect about half of runners annually. The frequencies of various RRI depend on the type of running, such as speed and mileage. Some injuries are acute, caused by sudden overstress, such as side stitch, strains, and sprains. Many of the common injuries that affect runners are chronic, developing over longer periods as the result of overuse. Common overuse injuries include shin splints, stress fractures, Achilles tendinitis, Iliotibial band syndrome, Patellofemoral pain, and plantar fasciitis.