Related Research Articles
Anesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general anesthetic. When it is used on specific nerve pathways, paralysis also can be achieved.

Sevoflurane, sold under the brand name Sevorane, among others, is a sweet-smelling, nonflammable, highly fluorinated methyl isopropyl ether used as an inhalational anaesthetic for induction and maintenance of general anesthesia. After desflurane, it is the volatile anesthetic with the fastest onset. While its offset may be faster than agents other than desflurane in a few circumstances, its offset is more often similar to that of the much older agent isoflurane. While sevoflurane is only half as soluble as isoflurane in blood, the tissue blood partition coefficients of isoflurane and sevoflurane are quite similar. For example, in the muscle group: isoflurane 2.62 vs. sevoflurane 2.57. In the fat group: isoflurane 52 vs. sevoflurane 50. As a result, the longer the case, the more similar will be the emergence times for sevoflurane and isoflurane.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Combined spinal and epidural anaesthesia (CSE) is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. The indwelling epidural catheter gives the ability to provide long lasting analgesia and to titrate the dose given to the desired effect.
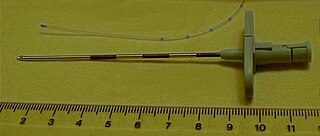
A Tuohy (/tOO-ee/) needle is a hollow hypodermic needle, very slightly curved at the end, suitable for inserting epidural catheters.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés. In the United States, over 50% of childbirths involve the use of epidural anesthesia.
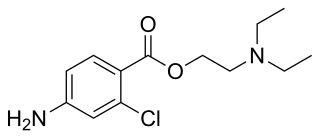
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.
Odom's indicator is a device used for locating the epidural space in regional anaesthesia. The device works on Dogliotti's principle by finding an area of decreased resistance to injection. It was originally designed on the assumption that the pressure in the epidural space was negative. This device is no-longer popular and alternative methods are now used.
Post-dural-puncture headache (PDPH) is a complication of puncture of the dura mater. The headache is severe and described as "searing and spreading like hot metal", involving the back and front of the head and spreading to the neck and shoulders, sometimes involving neck stiffness. It is exacerbated by movement and sitting or standing and is relieved to some degree by lying down. Nausea, vomiting, pain in arms and legs, hearing loss, tinnitus, vertigo, dizziness and paraesthesia of the scalp are also common.

An epidural blood patch (EBP) is a surgical procedure that uses autologous blood in order to close one or many holes in the dura mater of the spinal cord, usually as a result of a previous lumbar puncture or epidural. The procedure can be used to relieve orthostatic headaches, most commonly post dural puncture headache (PDPH). The procedure carries the typical risks of any epidural procedure. They are usually administered near the site of the cerebrospinal fluid leak, but in some cases the upper part of the spine is targeted. An epidural needle is inserted into the epidural space like a traditional epidural procedure. The blood modulates the pressure of the CSF and forms a clot, sealing the leak. EBPs were first described by American anesthesiologist Turan Ozdil and surgeon James B Gormley around 1960.
Cricoid pressure, also known as the Sellick manoeuvre or Sellick maneuver, is a technique used in endotracheal intubation to try to reduce the risk of regurgitation. The technique involves the application of pressure to the cricoid cartilage at the neck, thus occluding the esophagus which passes directly behind it.
Continuous wound infiltration (CWI) refers to the continuous infiltration of a local anesthetic into a surgical wound to aid in pain management during post-operative recovery.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.

Intravenous regional anesthesia (IVRA) or Bier's block anesthesia is an anesthetic technique on the body's extremities where a local anesthetic is injected intravenously and isolated from circulation in a target area. The technique usually involves exsanguination of the target region, which forces blood out of the extremity, followed by the application of pneumatic tourniquets to safely stop blood flow. The anesthetic agent is intravenously introduced into the limb and allowed to diffuse into the surrounding tissue while tourniquets retain the agent within the desired area.
The following outline is provided as an overview of and topical guide to anesthesia:
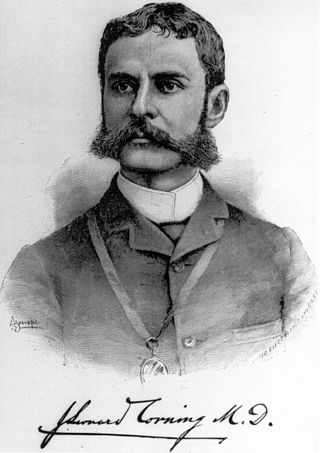
The history of neuraxial anesthesia goes back to 1885.

The laryngeal tube is an airway management device designed as an alternative to other airway management techniques such as mask ventilation, laryngeal mask airway, and tracheal intubation. This device can be inserted blindly through the oropharynx into the hypopharynx to create an airway during anaesthesia and cardiopulmonary resuscitation so as to enable mechanical ventilation of the lungs.
Fascia iliaca blocks is a local anesthetic nerve block, a type of regional anesthesia technique, used to provide analgesia or anaesthesia to the hip and thigh. FICB can performed by using ultrasound or with a loss of resistance technique, the latter sometimes referred to as the "two-pop-method". FICB works by affecting the femoral, obturator and the lateral cutaneous nerves with a local anesthetic.

Remifentanil acid is a metabolite of the potent short-acting synthetic opioid analgesic drug remifentanil. It is an analog of fentanyl and remifentanil.
References
- ↑ Dogliotti, AM (1933). "Research and clinical observations on spinal anesthesia: with special reference to the peridural technique" (PDF). Anesthesia & Analgesia . 12 (2): 59–65. doi:10.1213/00000539-193301000-00014. S2CID 70731119.
- ↑ Iklé A (July 1950). "Preliminary report of new technique for epidural anaesthesia". British Journal of Anaesthesia . 22 (3): 150–5. doi: 10.1093/bja/22.3.150 . PMID 15426701.
- 1 2 Wilson MJA (2007). "Epidural endeavour and the pressure principle". Anaesthesia. 62 (4): 319–324. doi: 10.1111/j.1365-2044.2007.05063.x . PMID 17381564.[ dead link ]
- ↑ Naulty JS, Ostheimer GW, Datta S, Knapp R, Weiss JB (November 1982). "Incidence of venous air embolism during epidural catheter insertion". Anesthesiology. 57 (5): 410–2. doi:10.1097/00000542-198211000-00010. PMID 7137620.
- ↑ Simopoulos T, Peeters-Asdourian C (June 2001). "Pneumocephalus after cervical epidural steroid injection". Anesth. Analg. 92 (6): 1576–7. doi:10.1097/00000539-200106000-00045. PMID 11375849. S2CID 42001070.