| Hypoprolactinemia | |
|---|---|
 | |
| Prolactin | |
| Specialty | Gynecology |
Hypoprolactinemia is a medical condition characterized by a deficiency in the serum levels of the hypothalamic-pituitary hormone prolactin. [1] [2]
| Hypoprolactinemia | |
|---|---|
 | |
| Prolactin | |
| Specialty | Gynecology |
Hypoprolactinemia is a medical condition characterized by a deficiency in the serum levels of the hypothalamic-pituitary hormone prolactin. [1] [2]
Hypoprolactinemia is associated with ovarian dysfunction in women, [3] [4] and, in men, metabolic syndrome, [5] anxiety symptoms, [5] arteriogenic erectile dysfunction, [6] premature ejaculation, [5] oligozoospermia (low concentration of sperm in semen), asthenospermia (reduced sperm motility), hypofunction of seminal vesicles, and hypoandrogenism. [7] In one study, normal sperm characteristics were restored when prolactin levels were brought up to normal values in men with hypoprolactinemia. [8] Hypoprolactinemia can be a cause of lactation failure after childbirth. [1] [9] [10]
Hypoprolactinemia can result from autoimmune disease, [2] hypopituitarism, [1] growth hormone deficiency, [2] hypothyroidism, [2] excessive dopamine action in the tuberoinfundibular pathway and/or the anterior pituitary, and ingestion of drugs that activate the D2 receptor, such as direct D2 receptor agonists like bromocriptine and pergolide, and indirect D2 receptor activators like amphetamines (through the induction of dopamine release). [11]
Guidelines for diagnosing hypoprolactinemia are defined as prolactin levels below 3 µg/L in women, [3] [4] and 5 µg/L in men. [12] [7] [8]
There are few treatments which increase prolactin levels in humans. Treatment differs based on the reason for diagnosis. Women who are diagnosed with hypoprolactinemia following lactation failure are typically advised to formula feed, although treatment with metoclopramide has been shown to increase milk supply in clinical studies. For subfertility, treatment may include clomiphene citrate or gonadotropins. [13]

Prolactin (PRL), also known as lactotropin and mammotropin, is a protein best known for its role in enabling mammals to produce milk. It is influential in over 300 separate processes in various vertebrates, including humans. Prolactin is secreted from the pituitary gland in response to eating, mating, estrogen treatment, ovulation and nursing. It is secreted heavily in pulses in between these events. Prolactin plays an essential role in metabolism, regulation of the immune system and pancreatic development.
Amenorrhea is the absence of a menstrual period in a female who has reached reproductive age. Physiological states of amenorrhoea are seen, most commonly, during pregnancy and lactation (breastfeeding). Outside the reproductive years, there is absence of menses during childhood and after menopause.

Hyperprolactinaemia is the presence of abnormally high levels of prolactin in the blood. Normal levels average to about 13 ng/mL in women, and 5 ng/mL in men, with an upper normal limit of serum prolactin levels being 15-25 ng/mL for both. When the fasting levels of prolactin in blood exceed this upper limit, hyperprolactinemia is indicated.
Growth hormone deficiency (GHD), or human growth hormone deficiency, is a medical condition resulting from not enough growth hormone (GH). Generally the most noticeable symptom is that an individual attains a short height. Newborns may also present low blood sugar or a small penis size. In adults there may be decreased muscle mass, high cholesterol levels, or poor bone density.
Anovulation is when the ovaries do not release an oocyte during a menstrual cycle. Therefore, ovulation does not take place. However, a woman who does not ovulate at each menstrual cycle is not necessarily going through menopause. Chronic anovulation is a common cause of infertility.
Hypogonadism means diminished functional activity of the gonads—the testicles or the ovaries—that may result in diminished production of sex hormones. Low androgen levels are referred to as hypoandrogenism and low estrogen as hypoestrogenism. These are responsible for the observed signs and symptoms in both males and females.

Hypopituitarism is the decreased (hypo) secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is known as selective hypopituitarism. If there is decreased secretion of most or all pituitary hormones, the term panhypopituitarism is used.

Pituitary adenomas are tumors that occur in the pituitary gland. Most pituitary tumors are benign, approximately 35% are invasive and just 0.1% to 0.2% are carcinomas. Pituitary adenomas represent from 10% to 25% of all intracranial neoplasms and the estimated prevalence rate in the general population is approximately 17%.
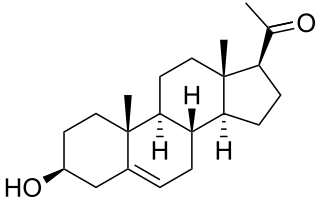
Pregnenolone (P5), or pregn-5-en-3β-ol-20-one, is an endogenous steroid and precursor/metabolic intermediate in the biosynthesis of most of the steroid hormones, including the progestogens, androgens, estrogens, glucocorticoids, and mineralocorticoids. In addition, pregnenolone is biologically active in its own right, acting as a neurosteroid.
Terms oligospermia, oligozoospermia, and low sperm count refer to semen with a low concentration of sperm and is a common finding in male infertility. Often semen with a decreased sperm concentration may also show significant abnormalities in sperm morphology and motility. There has been interest in replacing the descriptive terms used in semen analysis with more quantitative information.
Spermatogenesis arrest is known as the interruption of germinal cells of specific cellular type, which elicits an altered spermatozoa formation. Spermatogenic arrest is usually due to genetic factors resulting in irreversible azoospermia. However some cases may be consecutive to hormonal, thermic, or toxic factors and may be reversible either spontaneously or after a specific treatment. Spermatogenic arrest results in either oligospermia or azoospermia in men. It is quite a difficult condition to proactively diagnose as it tends to affect those who have normal testicular volumes; a diagnosis can be made however through a testicular biopsy.
The Ericsson method is an assisted reproductive technology for sex selection, used before implantation. In this method, sperm that will give rise to male versus female children are separated by moving at different speeds through a protein solution.

Homeobox protein prophet of PIT-1 is a protein that in humans is encoded by the PROP1 gene.

Luteinizing hormone subunit beta also known as lutropin subunit beta or LHβ is a polypeptide that in association with an alpha subunit common to all gonadotropin hormones forms the reproductive signaling molecule luteinizing hormone. In humans it is encoded by the LHB gene.
Hypomenorrhea or hypomenorrhoea, also known as short or scanty periods, is extremely light menstrual blood flow. It is the opposite of heavy periods or hypermenorrhea which is more properly called menorrhagia.
Sexual anhedonia, also known as pleasure dissociative orgasmic disorder, is a condition in which an individual cannot feel pleasure from an orgasm. It is thought to be a variant of hypoactive sexual desire disorder.
Hypogonadotropic hypogonadism (HH), is due to problems with either the hypothalamus or pituitary gland affecting the hypothalamic-pituitary-gonadal axis. Hypothalamic disorders result from a deficiency in the release of gonadotropic releasing hormone (GnRH), while pituitary gland disorders are due to a deficiency in the release of gonadotropins from the anterior pituitary. GnRH is the central regulator in reproductive function and sexual development via the HPG axis. GnRH is released by GnRH neurons, which are hypothalamic neuroendocrine cells, into the hypophyseal portal system acting on gonadotrophs in the anterior pituitary. The release of gonadotropins, LH and FSH, act on the gonads for the development and maintenance of proper adult reproductive physiology. LH acts on Leydig cells in the male testes and theca cells in the female. FSH acts on Sertoli cells in the male and follicular cells in the female. Combined this causes the secretion of gonadal sex steroids and the initiation of folliculogenesis and spermatogenesis. The production of sex steroids forms a negative feedback loop acting on both the anterior pituitary and hypothalamus causing a pulsatile secretion of GnRH. GnRH neurons lack sex steroid receptors and mediators such as kisspeptin stimulate GnRH neurons for pulsatile secretion of GnRH.
Androgen deficiency is a medical condition characterized by insufficient androgenic activity in the body. Androgen deficiency most commonly affects women, and is also called Female androgen insufficiency syndrome (FAIS), although it can happen in both sexes. Androgenic activity is mediated by androgens, and is dependent on various factors including androgen receptor abundance, sensitivity and function. Androgen deficiency is associated with lack of energy and motivation, depression, lack of desire (libido), and in more severe cases changes in secondary sex characteristics.

A prolactin modulator is a drug which affects the hypothalamic–pituitary–prolactin axis by modulating the secretion of the pituitary hormone prolactin from the anterior pituitary gland. Prolactin inhibitors suppress and prolactin releasers induce the secretion of prolactin, respectively.
The Postmenopausal Estrogen/Progestin Interventions (PEPI) trial was a large randomized controlled trial which assessed the influence of menopausal hormone therapy on cardiovascular and other outcomes.