Related Research Articles
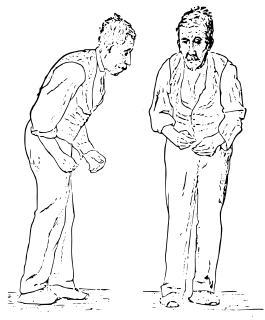
Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia, rigidity, and postural instability. These are the four motor symptoms found in Parkinson's disease (PD), after which it is named, dementia with Lewy bodies (DLB), Parkinson's disease dementia (PDD), and many other conditions. A wide range of causes may lead to this set of symptoms, including neurodegenerative conditions, drugs, toxins, metabolic diseases, and neurological conditions other than PD.

Dementia with Lewy bodies (DLB) is a type of dementia accompanied by changes in sleep, behavior, cognition, movement, and autonomic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive decline interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described by Kenji Kosaka in 1976.
Lewy body dementias describe two similar common dementias that are characterized by changes in thinking, movement, behavior, and mood. They are dementia with Lewy bodies (DLB), and Parkinson's disease dementia (PDD).

Rapid eye movement sleep behavior disorder or REM behavior disorder (RBD) is a sleep disorder in which people act out their dreams. It involves abnormal behavior during the sleep phase with rapid eye movement (REM) sleep. The major feature of RBD is loss of muscle atonia during otherwise intact REM sleep. REM sleep is the stage of sleep in which most vivid dreaming occurs. The loss of motor inhibition leads to a wide spectrum of behavioral release during sleep. This extends from simple limb twitches to more complex integrated movement. These behaviors can be violent in nature and in some cases will result in injury to either the individual or their bedmates.

Lewy bodies are the inclusion bodies – abnormal aggregations of protein – that develop inside nerve cells affected by Parkinson's disease (PD), the Lewy body dementias, and some other disorders. They are also seen in cases of multiple system atrophy, particularly the parkinsonian variant (MSA-P).

Multiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by autonomic dysfunction, tremors, slow movement, muscle rigidity, and postural instability and ataxia. This is caused by progressive degeneration of neurons in several parts of the brain including the basal ganglia, inferior olivary nucleus, and cerebellum.
Degenerative disease is the result of a continuous process based on degenerative cell changes, affecting tissues or organs, which will increasingly deteriorate over time.
Progressive supranuclear palsy (PSP) is a late-onset degenerative disease involving the gradual deterioration and death of specific volumes of the brain. The condition leads to symptoms including loss of balance, slowing of movement, difficulty moving the eyes, and dementia. PSP may be mistaken for other neurodegenerative diseases such as Parkinson's and Alzheimer's. The cause of the condition is uncertain, but involves accumulation of tau protein within the brain. Medications such as levodopa and amantadine may be useful in some cases.
Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and the average disease duration is six years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.

Tauopathy belongs to a class of neurodegenerative diseases involving the aggregation of tau protein into neurofibrillary or gliofibrillary tangles (NFTs) in the human brain. Tangles are formed by hyperphosphorylation of the microtubule protein known as tau, causing the protein to dissociate from microtubules and form insoluble aggregates. The mechanism of tangle formation is not well understood, and whether tangles are a primary cause of Alzheimer's disease or play a peripheral role is unknown.

Frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17) is an autosomal dominant neurodegenerative tauopathy and Parkinson plus syndrome. FTDP-17 is caused by mutations in the MAPT gene located on the q arm of chromosome 17, and has three cardinal features: behavioral and personality changes, cognitive impairment, and motor symptoms. FTDP-17 was defined during the International Consensus Conference in Ann Arbor, Michigan, in 1996.
Subcortical dementias includes those diseases which predominantly affects the basal ganglia along with features of cognitive decline.

Parkinson's disease (PD), or simply Parkinson's is a long-term degenerative disorder of the central nervous system that mainly affects the motor system. The symptoms usually emerge slowly and, as the disease worsens, non-motor symptoms become more common. The most obvious early symptoms are tremor, rigidity, slowness of movement, and difficulty with walking, but cognitive and behavioral problems may also occur. Parkinson's disease dementia becomes common in the advanced stages of the disease. Depression and anxiety are also common, occurring in more than a third of people with PD. Other symptoms include sensory, sleep, and emotional problems. The main motor symptoms are collectively called "parkinsonism", or a "parkinsonian syndrome".

Signs and symptoms of Parkinson's disease are varied. Parkinson's disease affects movement, producing motor symptoms. Non-motor symptoms, which include dysautonomia, cognitive and neurobehavioral problems, and sensory and sleep difficulties, are also common. When other diseases mimic Parkinson's disease, they are categorized as parkinsonism.
Kufor–Rakeb syndrome is an autosomal recessive disorder of juvenile onset also known as Parkinson disease-9 (PARK9).

The history of Parkinson's disease expands from 1817, when British apothecary James Parkinson published An Essay on the Shaking Palsy, to modern times. Before Parkinson's descriptions, others had already described features of the disease that would bear his name, while the 20th century greatly improved knowledge of the disease and its treatments. PD was then known as paralysis agitans. The term "Parkinson's disease" was coined in 1865 by William Sanders and later popularized by French neurologist Jean-Martin Charcot. Paralysis
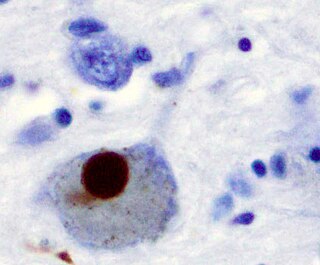
Synucleinopathies are neurodegenerative diseases characterised by the abnormal accumulation of aggregates of alpha-synuclein protein in neurons, nerve fibres or glial cells. There are three main types of synucleinopathy: Parkinson's disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). Other rare disorders, such as various neuroaxonal dystrophies, also have α-synuclein pathologies.
Parkinson's disease dementia (PDD) is dementia that is associated with Parkinson's disease (PD). Together with dementia with Lewy bodies (DLB), it is one of the Lewy body dementias characterized by abnormal deposits of Lewy bodies in the brain.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and a type of frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.
The Frontal Assessment Battery (FAB), is a short screening test to evaluate executive function (EF).
References
- ↑ Bensimon G, Ludolph A, Agid Y, Vidailhet M, Payan C, Leigh PN (January 2009). "Riluzole treatment, survival and diagnostic criteria in Parkinson plus disorders: the NNIPPS study". Brain. 132 (Pt 1): 156–71. doi:10.1093/brain/awn291. PMC 2638696 . PMID 19029129.
- ↑ Cecil Textbook of Medicine, 22nd edition, ISBN 0-7216-9652-X
- 1 2 3 4 Mitra K.; Gangopadhaya P. K.; Das S. K. (2003). "Parkinsonism plus syndrome—a review". Neurol India. 51 (2): 183–188. PMID 14570999.
- ↑ Mark, M. H. (2001). "Lumping and splitting the Parkinson Plus syndromes: dementia with Lewy bodies, multiple system atrophy, progressive supranuclear palsy, and cortical-basal ganglionic degeneration". Neurologic Clinics. 19 (3): 607–27. doi:10.1016/S0733-8619(05)70037-2. PMID 11532646.
- ↑ Levin J, Kurz A, Arzberger T, Giese A, Höglinger GU (February 5, 2016). "The Differential Diagnosis and Treatment of Atypical Parkinsonism". Dtsch Arztebl Int. 113 (5): 61–9. doi:10.3238/arztebl.2016.0061. PMC 4782269 . PMID 26900156.
- ↑ Brittany N. Dugger; Charles H. Adler; Holly A. Shill; John Caviness; Sandra Jacobson; Erika Driver-Dunckley; Thomas G. Beach & the Arizona Parkinson’s Disease Consortium (May 2014). "Concomitant pathologies among a spectrum of parkinsonian disorders". Parkinsonism Relat Disord. 20 (5): 525–9. doi:10.1016/j.parkreldis.2014.02.012. PMC 4028418 . PMID 24637124.
- ↑ Constance Ward (2006). "Characteristics and symptom management of progressive supranuclear palsy: a multidisciplinary approach" (PDF). Journal of Neuroscience Nursing. 38 (4): 242–247. doi:10.1097/01376517-200608000-00007. PMID 16925000. Archived from the original (PDF) on 2008-07-23.
- ↑ "Multiple System Atrophy with Orthostatic Hypotension Information Page". Archived from the original on 2012-05-14. Retrieved 2009-09-15.
- ↑ Hierholzer, Johannes; Cordes, Michael; Venz, Stephan; Schelosky, Ludwig; Harisch, Cordula; Richter, Wolf; Keske, Uwe; Hosten, Norbert; Mäurer, Jürgen (1998-06-01). "Loss of Dopamine-D2 Receptor Binding Sites in Parkinsonian Plus Syndromes". Journal of Nuclear Medicine. 39 (6): 954–960. ISSN 0161-5505. PMID 9627325.
- ↑ Litvan I, Campbell G, Mangone CA, Verny M, McKee A, Chaudhuri KR, Jellinger K, Pearce RK, D'Olhaberriague L (Jan 1997). "Which clinical features differentiate progressive supranuclear palsy (Steele-Richardson-Olzewski syndrome) from related disorders". Brain. 120 (1): 65–74. doi: 10.1093/brain/120.1.65 . PMID 9055798.
- ↑ David R. Williams & Irene Litvan (October 2013). "Parkinsonian syndromes". Continuum (Minneap Minn). 19 (5 Movement Disorders): 1189–212. doi:10.1212/01.CON.0000436152.24038.e0. PMC 4234134 . PMID 24092286.
- ↑ Molloy, F. M., & Healy, D. G. (2011). Parkinsonism Plus Syndromes. In O. Hardiman & C. P. Doherty (Eds.), Neurodegenerative Disorders (181-196). London: Springer London. doi : 10.1007/978-1-84996-011-3_9
- ↑ Ling H (2016). "Clinical Approach to Progressive Supranuclear Palsy". J Mov Disord. 9 (1): 3–13. doi:10.14802/jmd.15060. PMC 4734991 . PMID 26828211.
- ↑ Milestones in Atypical and Secondary Parkinsonisms