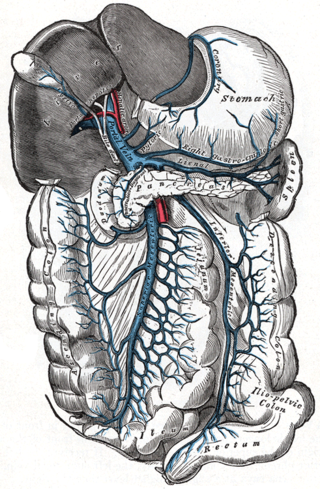
In human anatomy, the mesentery, an organ that attaches the intestines to the posterior abdominal wall, comprises the double fold of the peritoneum. It helps in storing fat and allowing blood vessels, lymphatics, and nerves to supply the intestines.
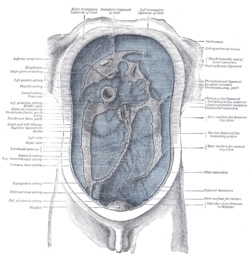
The rectouterine pouch is the extension of the peritoneum into the space between the posterior wall of the uterus and the rectum in the human female.

The celiacartery, also known as the celiac trunk or truncus coeliacus, is the first major branch of the abdominal aorta. It is about 1.25 cm in length. Branching from the aorta at thoracic vertebra 12 (T12) in humans, it is one of three anterior/ midline branches of the abdominal aorta.
In human anatomy, the superior mesenteric artery (SMA) is an artery which arises from the anterior surface of the abdominal aorta, just inferior to the origin of the celiac trunk, and supplies blood to the intestine from the lower part of the duodenum through two-thirds of the transverse colon, as well as the pancreas.

In human anatomy, the inferior mesenteric artery (IMA) is the third main branch of the abdominal aorta and arises at the level of L3, supplying the large intestine from the distal transverse colon to the upper part of the anal canal. The regions supplied by the IMA are the descending colon, the sigmoid colon, and part of the rectum.
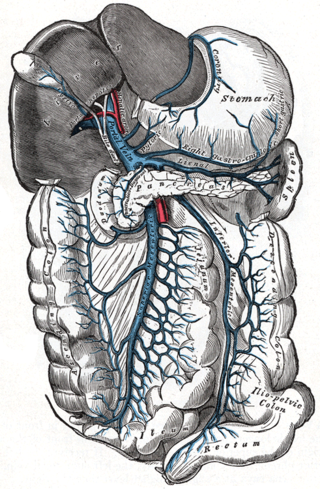
In human anatomy, the inferior mesenteric vein (IMV) is a blood vessel that drains blood from the large intestine. It usually terminates when reaching the splenic vein, which goes on to form the portal vein with the superior mesenteric vein (SMV).

The lesser omentum is the double layer of peritoneum that extends from the liver to the lesser curvature of the stomach, and to the first part of the duodenum. The lesser omentum is usually divided into these two connecting parts: the hepatogastric ligament, and the hepatoduodenal ligament.
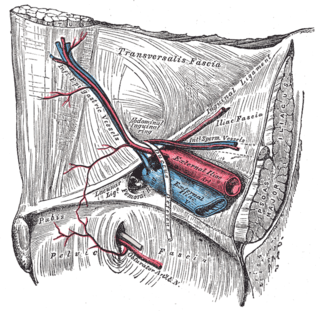
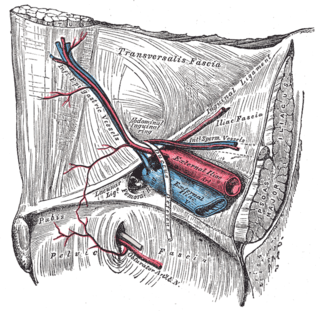
In human anatomy, the inferior epigastric artery is an artery that arises from the external iliac artery. It is accompanied by the inferior epigastric vein; inferiorly, these two inferior epigastric vessels together travel within the lateral umbilical fold The inferior epigastric artery then traverses the arcuate line of rectus sheath to enter the rectus sheath, then anastomoses with the superior epigastric artery within the rectus sheath.

also known as superior tendon of abdominal cavity.

The middle colic artery is an artery of the abdomen; a branch of the superior mesenteric artery distributed to parts of the ascending and transverse colon. It usually divides into two terminal branches - a left one and a right one - which go on to form anastomoses with the left colic artery, and right colic artery (respectively), thus participating in the formation of the marginal artery of the colon.

The left colic artery is a branch of the inferior mesenteric artery distributed to the descending colon, and left part of the transverse colon. It ends by dividing into an ascending branch and a descending branch; the terminal branches of the two branches go on to form anastomoses with the middle colic artery, and a sigmoid artery (respectively).

In the anatomy of the human digestive tract, there are two colic flexures, or curvatures in the transverse colon. The right colic flexure is also known as the hepatic flexure, and the left colic flexure is also known as the splenic flexure. Note that "right" refers to the patient's anatomical right, which may be depicted on the left of a diagram.

The greater omentum is a large apron-like fold of visceral peritoneum that hangs down from the stomach. It extends from the greater curvature of the stomach, passing in front of the small intestines and doubles back to ascend to the transverse colon before reaching to the posterior abdominal wall. The greater omentum is larger than the lesser omentum, which hangs down from the liver to the lesser curvature. The common anatomical term "epiploic" derives from "epiploon", from the Greek epipleein, meaning to float or sail on, since the greater omentum appears to float on the surface of the intestines. It is the first structure observed when the abdominal cavity is opened anteriorly.

The duodenojejunal flexure or duodenojejunal junction, also known as the angle of Treitz, is the border between the duodenum and the jejunum.

The suspensory ligament of the ovary, also infundibulopelvic ligament, is a fold of peritoneum that extends out from the ovary to the wall of the pelvis.

The lateral umbilical fold is an elevation of the peritoneum lining the inner/posterior surface of the lower anterior abdominal wall formed by the underlying inferior epigastric artery and inferior epigastric vein which the peritoneum covers. Superiorly, the lateral umbilical fold ends where the vessels reach and enter the rectus sheath at the arcuate line of rectus sheath; in spite of the name, the lateral umbilical folds do not extend as far superiorly as the umbilicus. Inferiorly, it extends to just medial to the deep inguinal ring.
The paracolic gutters are peritoneal recesses – spaces between the colon and the abdominal wall.

The gastrosplenic ligament is part of the greater omentum extending between the stomach and the spleen. It contains several blood vessels.

In human anatomy, the omental foramen is the passage of communication, or foramen, between the greater sac, and the lesser sac of the peritoneal cavity.

The paramesenteric gutters are two peritoneal recesses – spaces in the abdominal cavity between the colon and the root of the mesentery. There are two paramesenteric gutters; the left paramesenteric gutter and the right paramesenteric gutter.