| Peyronie's disease | |
|---|---|
| Other names | Peyronie disease, induratio penis plastica (IPP), [1] chronic inflammation of the tunica albuginea (CITA) |
 | |
| Man showing abnormal curvature of the penis associated with Peyronie's disease | |
| Pronunciation | |
| Specialty | Urology |
| Causes | Unknown [2] |
| Frequency | ~10% of men [2] |
| Named after | François Gigot de la Peyronie |
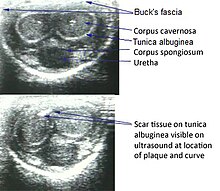
Peyronie's disease is a connective tissue disorder involving the growth of fibrous plaques in the soft tissue of the penis. Specifically, scar tissue forms in the tunica albuginea, the thick sheath of tissue surrounding the corpora cavernosa, causing pain, abnormal curvature, erectile dysfunction, indentation, loss of girth and shortening. [2] [3]
Contents
- Signs and symptoms
- Psychosocial
- Causes
- Diagnosis
- Ultrasonography
- Treatment
- Medication and supplements
- Physical therapy and devices
- Surgery
- Epidemiology
- History
- References
- External links
It is estimated to affect 1–20% of men. [2] The condition becomes more common with age. [2]