Radiation therapy or radiotherapy is a treatment using ionizing radiation, generally provided as part of cancer therapy to either kill or control the growth of malignant cells. It is normally delivered by a linear particle accelerator. Radiation therapy may be curative in a number of types of cancer if they are localized to one area of the body, and have not spread to other parts. It may also be used as part of adjuvant therapy, to prevent tumor recurrence after surgery to remove a primary malignant tumor. Radiation therapy is synergistic with chemotherapy, and has been used before, during, and after chemotherapy in susceptible cancers. The subspecialty of oncology concerned with radiotherapy is called radiation oncology. A physician who practices in this subspecialty is a radiation oncologist.

External beam radiation therapy (EBRT) is a form of radiotherapy that utilizes a high-energy collimated beam of ionizing radiation, from a source outside the body, to target and kill cancer cells. A radiotherapy beam is composed of particles which travel in a consistent direction; each radiotherapy beam consists of one type of particle intended for use in treatment, though most beams contain some contamination by other particle types.

Brachytherapy is a form of radiation therapy where a sealed radiation source is placed inside or next to the area requiring treatment. Brachy is Greek for short. Brachytherapy is commonly used as an effective treatment for cervical, prostate, breast, esophageal and skin cancer and can also be used to treat tumours in many other body sites. Treatment results have demonstrated that the cancer-cure rates of brachytherapy are either comparable to surgery and external beam radiotherapy (EBRT) or are improved when used in combination with these techniques. Brachytherapy can be used alone or in combination with other therapies such as surgery, EBRT and chemotherapy.
The Therac-25 is a computer-controlled radiation therapy machine produced by Atomic Energy of Canada Limited (AECL) in 1982 after the Therac-6 and Therac-20 units.
Radiation protection, also known as radiological protection, is defined by the International Atomic Energy Agency (IAEA) as "The protection of people from harmful effects of exposure to ionizing radiation, and the means for achieving this". Exposure can be from a source of radiation external to the human body or due to internal irradiation caused by the ingestion of radioactive contamination.

In medicine, proton therapy, or proton radiotherapy, is a type of particle therapy that uses a beam of protons to irradiate diseased tissue, most often to treat cancer. The chief advantage of proton therapy over other types of external beam radiotherapy is that the dose of protons is deposited over a narrow range of depth; hence in minimal entry, exit, or scattered radiation dose to healthy nearby tissues.

Radiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. Like other forms of radiation therapy, it is usually used to treat cancer. Radiosurgery was originally defined by the Swedish neurosurgeon Lars Leksell as "a single high dose fraction of radiation, stereotactically directed to an intracranial region of interest".
A monitor unit (MU) is a measure of machine output from a clinical accelerator for radiation therapy such as a linear accelerator or an orthovoltage unit. Monitor units are measured by monitor chambers, which are ionization chambers that measure the dose delivered by a beam and are built into the treatment head of radiotherapy linear accelerators.
The ionization chamber is the simplest type of gaseous ionisation detector, and is widely used for the detection and measurement of many types of ionizing radiation, including X-rays, gamma rays, alpha particles and beta particles. Conventionally, the term "ionization chamber" refers exclusively to those detectors which collect all the charges created by direct ionization within the gas through the application of an electric field. It uses the discrete charges created by each interaction between the incident radiation and the gas to produce an output in the form of a small direct current. This means individual ionising events cannot be measured, so the energy of different types of radiation cannot be differentiated, but it gives a very good measurement of overall ionising effect.

A radiation burn is a damage to the skin or other biological tissue and organs as an effect of radiation. The radiation types of greatest concern are thermal radiation, radio frequency energy, ultraviolet light and ionizing radiation.

Fast neutron therapy utilizes high energy neutrons typically between 50 and 70 MeV to treat cancer. Most fast neutron therapy beams are produced by reactors, cyclotrons (d+Be) and linear accelerators. Neutron therapy is currently available in Germany, Russia, South Africa and the United States. In the United States, one treatment center is operational, in Seattle, Washington. The Seattle center uses a cyclotron which produces a proton beam impinging upon a beryllium target.

In radiotherapy, radiation treatment planning (RTP) is the process in which a team consisting of radiation oncologists, radiation therapist, medical physicists and medical dosimetrists plan the appropriate external beam radiotherapy or internal brachytherapy treatment technique for a patient with cancer.
Electron therapy or electron beam therapy (EBT) is a kind of external beam radiotherapy where electrons are directed to a tumor site for medical treatment of cancer.
Intraoperative radiation therapy (IORT) is radiation therapy that is administered during surgery directly in the operating room.
Particle therapy is a form of external beam radiotherapy using beams of energetic neutrons, protons, or other heavier positive ions for cancer treatment. The most common type of particle therapy as of August 2021 is proton therapy.
In medicine, a bolus is the administration of a discrete amount of medication, drug, or other compound within a specific time, generally 1–30 minutes, to raise its concentration in blood to an effective level. The administration can be given by injection: intravenously, intramuscularly, intrathecally, subcutaneously, or by inhalation. The article on routes of administration provides more information, as the preceding list of ROAs is not exhaustive.
Intraoperative electron radiation therapy is the application of electron radiation directly to the residual tumor or tumor bed during cancer surgery. Electron beams are useful for intraoperative radiation treatment because, depending on the electron energy, the dose falls off rapidly behind the target site, therefore sparing underlying healthy tissue.
The Deep-dose equivalent (DDE) is a measure of external radiation exposure defined by US regulations. It is reported alongside eye and shallow dose equivalents on typical US dosimetry reports. It represents the dose equivalent at a tissue depth of 1 cm (1000 mg/cm2) due to external whole-body exposure to ionizing radiation.
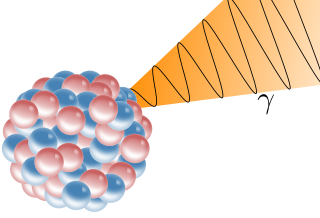
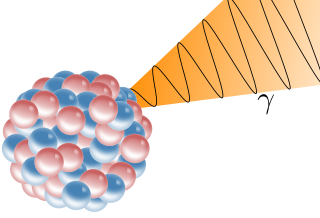
A gamma ray, also known as gamma radiation (symbol
γ
), is a penetrating form of electromagnetic radiation arising from the radioactive decay of atomic nuclei. It consists of the shortest wavelength electromagnetic waves, typically shorter than those of X-rays. With frequencies above 30 exahertz (3×1019 Hz) and wavelength less than 10 picometer (1×10−11 m) gamma ray photons have the highest photon energy of any form of electromagnetic radiation. Paul Villard, a French chemist and physicist, discovered gamma radiation in 1900 while studying radiation emitted by radium. In 1903, Ernest Rutherford named this radiation gamma rays based on their relatively strong penetration of matter; in 1900 he had already named two less penetrating types of decay radiation (discovered by Henri Becquerel) alpha rays and beta rays in ascending order of penetrating power.
A beam spoiler is a piece of material, placed into the path of the photon beam in radiotherapy. The purpose of the spoiler is to reduce the depth of the maximum radiation dosage.