The urea breath test is a rapid diagnostic procedure used to identify infections by Helicobacter pylori, a spiral bacterium implicated in gastritis, gastric ulcer, and peptic ulcer disease. It is based upon the ability of H. pylori to convert urea to ammonia and carbon dioxide. Urea breath tests are recommended in leading society guidelines as a preferred non-invasive choice for detecting H. pylori before and after treatment.

Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, flagellated, helical bacterium. Mutants can have a rod or curved rod shape, and these are less effective. Its helical body is thought to have evolved in order to penetrate the mucous lining of the stomach, helped by its flagella, and thereby establish infection. The bacterium was first identified as the causal agent of gastric ulcers in 1983 by the Australian doctors Barry Marshall and Robin Warren.

Helicobacter is a genus of gram-negative bacteria possessing a characteristic helical shape. They were initially considered to be members of the genus Campylobacter, but in 1989, Goodwin et al. published sufficient reasons to justify the new genus name Helicobacter. The genus Helicobacter contains about 35 species.

Staining is a technique used to enhance contrast in samples, generally at the microscopic level. Stains and dyes are frequently used in histology, in cytology, and in the medical fields of histopathology, hematology, and cytopathology that focus on the study and diagnoses of diseases at the microscopic level. Stains may be used to define biological tissues, cell populations, or organelles within individual cells.

Gastritis is inflammation of the lining of the stomach. It may occur as a short episode or may be of a long duration. There may be no symptoms but, when symptoms are present, the most common is upper abdominal pain. Other possible symptoms include nausea and vomiting, bloating, loss of appetite and heartburn. Complications may include stomach bleeding, stomach ulcers, and stomach tumors. When due to autoimmune problems, low red blood cells due to not enough vitamin B12 may occur, a condition known as pernicious anemia.

Acid-fastness is a physical property of certain bacterial and eukaryotic cells, as well as some sub-cellular structures, specifically their resistance to decolorization by acids during laboratory staining procedures. Once stained as part of a sample, these organisms can resist the acid and/or ethanol-based decolorization procedures common in many staining protocols, hence the name acid-fast.

Atrophic gastritis is a process of chronic inflammation of the gastric mucosa of the stomach, leading to a loss of gastric glandular cells and their eventual replacement by intestinal and fibrous tissues. As a result, the stomach's secretion of essential substances such as hydrochloric acid, pepsin, and intrinsic factor is impaired, leading to digestive problems. The most common are vitamin B12 deficiency possibly leading to pernicious anemia; and malabsorption of iron, leading to iron deficiency anaemia. It can be caused by persistent infection with Helicobacter pylori, or can be autoimmune in origin. Those with autoimmune atrophic gastritis (Type A gastritis) are statistically more likely to develop gastric carcinoma, Hashimoto's thyroiditis, and achlorhydria.

A microaerophile is a microorganism that requires environments containing lower levels of dioxygen than that are present in the atmosphere (i.e. < 21% O2; typically 2–10% O2) for optimal growth. A more restrictive interpretation requires the microorganism to be obligate in this requirement. Many microaerophiles are also capnophiles, requiring an elevated concentration of carbon dioxide (e.g. 10% CO2 in the case of Campylobacter species).
The oxidase test is used to determine whether an organism possesses the cytochrome c oxidase enzyme. The test is used as an aid for the differentiation of Neisseria, Moraxella, Campylobacter and Pasteurella species. It is also used to differentiate pseudomonads from related species.
MALT lymphoma is a form of lymphoma involving the mucosa-associated lymphoid tissue (MALT), frequently of the stomach, but virtually any mucosal site can be affected. It is a cancer originating from B cells in the marginal zone of the MALT.

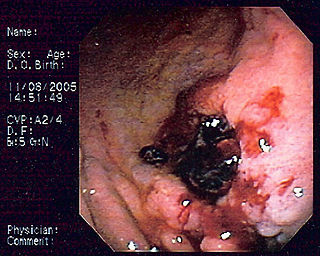
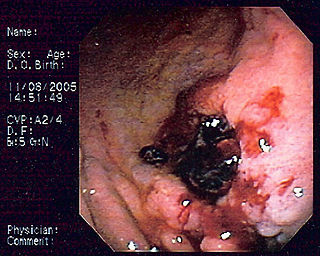
Rapid urease test, also known as the CLO test, is a rapid diagnostic test for diagnosis of Helicobacter pylori. The basis of the test is the ability of H. pylori to secrete the urease enzyme, which catalyzes the conversion of urea to ammonia and carbon dioxide.

This is a timeline of the events relating to the discovery that peptic ulcer disease and some cancers are caused by H. pylori. In 2005, Barry Marshall and Robin Warren were awarded the Nobel Prize in Physiology or Medicine for their discovery that peptic ulcer disease (PUD) was primarily caused by Helicobacter pylori, a bacterium with affinity for acidic environments, such as the stomach. As a result, PUD that is associated with H. pylori is currently treated with antibiotics used to eradicate the infection. For decades prior to their discovery, it was widely believed that PUD was caused by excess acid in the stomach. During this time, acid control was the primary method of treatment for PUD, to only partial success. Among other effects, it is now known that acid suppression alters the stomach milieu to make it less amenable to H. pylori infection.

Duodenitis is inflammation of the duodenum. It may persist acutely or chronically.

Cancer bacteria are bacteria infectious organisms that are known or suspected to cause cancer. While cancer-associated bacteria have long been considered to be opportunistic, there is some evidence that bacteria may be directly carcinogenic. The strongest evidence to date involves the bacterium H. pylori and its role in gastric cancer.
Helicobacter pylori eradication protocols is a standard name for all treatment protocols for peptic ulcers and gastritis in the presence of Helicobacter pylori infection. The primary goal of the treatment is not only temporary relief of symptoms but also total elimination of H. pylori infection. Patients with active duodenal or gastric ulcers and those with a prior ulcer history should be tested for H. pylori. Appropriate therapy should be given for eradication. Patients with MALT lymphoma should also be tested and treated for H. pylori since eradication of this infection can induce remission in many patients when the tumor is limited to the stomach. Several consensus conferences, including the Maastricht Consensus Report, recommend testing and treating several other groups of patients but there is limited evidence of benefit. This includes patients diagnosed with gastric adenocarcinoma, patients found to have atrophic gastritis or intestinal metaplasia, as well as first-degree relatives of patients with gastric adenocarcinoma since the relatives themselves are at increased risk of gastric cancer partly due to the intrafamilial transmission of H. pylori. To date, it remains controversial whether to test and treat all patients with functional dyspepsia, gastroesophageal reflux disease, or other non-GI disorders as well as asymptomatic individuals.

Marginal zone lymphomas, also known as marginal zone B-cell lymphomas (MZLs), are a heterogeneous group of lymphomas that derive from the malignant transformation of marginal zone B-cells. Marginal zone B cells are innate lymphoid cells that normally function by rapidly mounting IgM antibody immune responses to antigens such as those presented by infectious agents and damaged tissues. They are lymphocytes of the B-cell line that originate and mature in secondary lymphoid follicles and then move to the marginal zones of mucosa-associated lymphoid tissue (MALT), the spleen, or lymph nodes. Mucosa-associated lymphoid tissue is a diffuse system of small concentrations of lymphoid tissue found in various submucosal membrane sites of the body such as the gastrointestinal tract, mouth, nasal cavity, pharynx, thyroid gland, breast, lung, salivary glands, eye, skin and the human spleen.

Helicobacter cinaedi is a bacterium in the family Helicobacteraceae, Campylobacterales order, Helicobacteraceae family, Helicobacter genus. It was formerly known as Campylobacter cinaedi until molecular analysis published in 1991 led to a major revision of the genus Campylobacter. H. cinaedi is a curved, spiral, or fusiform rod with flagellum at both of its ends which it uses to dart around. The bacterium is a pathogen.

The Warthin–Starry stain (WS) is a silver nitrate-based staining method used in histology. It was first introduced in 1920 by American pathologists Aldred Scott Warthin (1866–1931) and Allen Chronister Starry (1890–1973), for the detection of spirochetes. It has been considered a standard stain for the detection of spirochetes, and is also used to stain Helicobacter pylori, Lawsonia intracellularis, Microsporidia, and particulates. It is also important for confirmation of Bartonella henselae, a causative organism in cat-scratch disease.
Spiral bacteria, bacteria of spiral (helical) shape, form the third major morphological category of prokaryotes along with the rod-shaped bacilli and round cocci. Spiral bacteria can be subclassified by the number of twists per cell, cell thickness, cell flexibility, and motility. The two types of spiral cells are spirillum and spirochete, with spirillum being rigid with external flagella, and spirochetes being flexible with internal flagella.
The genus Wolinella is a member of the Campylobacterales order of Bacteria. The order Campylobacterales includes human pathogens such as Helicobacter pylori and Campylobacter jejuni.