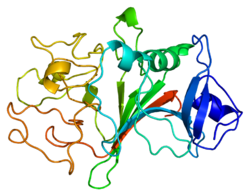
1fib: RECOMBINANT HUMAN GAMMA-FIBRINOGEN CARBOXYL TERMINAL FRAGMENT (RESIDUES 143-411) BOUND TO CALCIUM AT PH 6.0
1fic: STRUCTURE OF HUMAN GAMMA FIBRINOGEN 30 KD CARBOXYL TERMINAL FRAGMENT
1fid: STRUCTURE OF HUMAN GAMMA FIBRINOGEN 30 KD CARBOXYL TERMINAL FRAGMENT
1fza: CRYSTAL STRUCTURE OF FIBRINOGEN FRAGMENT D
1fzb: CRYSTAL STRUCTURE OF CROSSLINKED FRAGMENT D
1fzc: CRYSTAL STRUCTURE OF FRAGMENT DOUBLE-D FROM HUMAN FIBRIN WITH TWO DIFFERENT BOUND LIGANDS
1fze: CRYSTAL STRUCTURE OF FRAGMENT DOUBLE-D FROM HUMAN FIBRIN
1fzf: CRYSTAL STRUCTURE OF FRAGMENT DOUBLE-D FROM HUMAN FIBRIN WITH THE PEPTIDE LIGAND GLY-HIS-ARG-PRO-AMIDE
1fzg: CRYSTAL STRUCTURE OF FRAGMENT D FROM HUMAN FIBRINOGEN WITH THE PEPTIDE LIGAND GLY-HIS-ARG-PRO-AMIDE
1lt9: Crystal Structure of Recombinant Human Fibrinogen Fragment D
1ltj: Crystal Structure of Recombinant Human Fibrinogen Fragment D with the Peptide Ligands Gly-Pro-Arg-Pro-Amide and Gly-His-Arg-Pro-Amide
1n86: Crystal structure of human D-dimer from cross-linked fibrin complexed with GPR and GHRPLDK peptide ligands.
1n8e: Fragment Double-D from Human Fibrin
1re3: Crystal Structure of Fragment D of BbetaD398A Fibrinogen with the Peptide Ligand Gly-His-Arg-Pro-Amide
1re4: Crystal Structure of Fragment D of BbetaD398A Fibrinogen
1rf0: Crystal Structure of Fragment D of gammaE132A Fibrinogen
1rf1: Crystal Structure of Fragment D of gammaE132A Fibrinogen with the Peptide Ligand Gly-His-Arg-Pro-amide
2a45: Crystal structure of the complex between thrombin and the central ""E"" region of fibrin
2ffd: Fibrinogen Fragment D with ""A"" knob peptide mimic GPRVVE
2fib: RECOMBINANT HUMAN GAMMA-FIBRINOGEN CARBOXYL TERMINAL FRAGMENT (RESIDUES 143-411) COMPLEXED TO THE PEPTIDE GLY-PRO-ARG-PRO AT PH 6.0
2h43: Crystal Structure of Human Fragment D Complexed with Ala-His-Arg-Pro-amide
2hod: Crystal Structure of Fragment D from Human Fibrinogen Complexed with Gly-hydroxyPro-Arg-Pro-amide
2hpc: Crystal structure of fragment D from Human Fibrinogen Complexed with Gly-Pro-Arg-Pro-amide.
2oyh: Crystal Structure of Fragment D of gammaD298,301A Fibrinogen with the Peptide Ligand Gly-His-Arg-Pro-Amide
2oyi: Crystal Structure of Fragment D of gammaD298,301A Fibrinogen with the Peptide Ligand Gly-Pro-Arg-Pro-Amide
3fib: RECOMBINANT HUMAN GAMMA-FIBRINOGEN CARBOXYL TERMINAL FRAGMENT (RESIDUES 143-411) BOUND TO CALCIUM AT PH 6.0: A FURTHER REFINEMENT OF PDB ENTRY 1FIB, AND DIFFERS FROM 1FIB BY THE MODELLING OF A CIS PEPTIDE BOND BETWEEN RESIDUES K338 AND C339