The stomach is a muscular, hollow organ in the gastrointestinal tract of humans and many other animals, including several invertebrates. The stomach has a dilated structure and functions as a vital organ in the digestive system. The stomach is involved in the gastric phase of digestion, following chewing. It performs a chemical breakdown by means of enzymes and hydrochloric acid.

Digestion is the breakdown of large insoluble food compounds into small water-soluble components so that they can be absorbed into the blood plasma. In certain organisms, these smaller substances are absorbed through the small intestine into the blood stream. Digestion is a form of catabolism that is often divided into two processes based on how food is broken down: mechanical and chemical digestion. The term mechanical digestion refers to the physical breakdown of large pieces of food into smaller pieces which can subsequently be accessed by digestive enzymes. Mechanical digestion takes place in the mouth through mastication and in the small intestine through segmentation contractions. In chemical digestion, enzymes break down food into the small compounds that the body can use.
Chyme or chymus is the semi-fluid mass of partly digested food that is expelled by a person's or another animal's stomach, through the pyloric valve, into the duodenum.

Zollinger–Ellison syndrome is rare disease in which tumors cause the stomach to produce too much acid, resulting in peptic ulcers. Symptoms include abdominal pain and diarrhea.

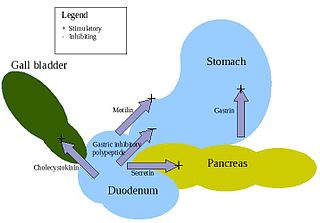
Cholecystokinin is a peptide hormone of the gastrointestinal system responsible for stimulating the digestion of fat and protein. Cholecystokinin, formerly called pancreozymin, is synthesized and secreted by enteroendocrine cells in the duodenum, the first segment of the small intestine. Its presence causes the release of digestive enzymes and bile from the pancreas and gallbladder, respectively, and also acts as a hunger suppressant.

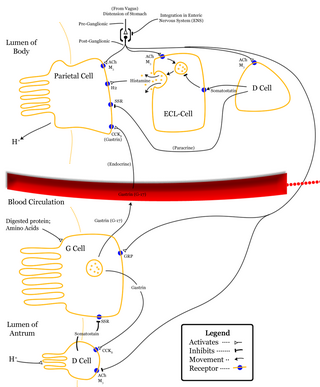
Gastrin is a peptide hormone that stimulates secretion of gastric acid (HCl) by the parietal cells of the stomach and aids in gastric motility. It is released by G cells in the pyloric antrum of the stomach, duodenum, and the pancreas.

Parietal cells (also known as oxyntic cells) are epithelial cells in the stomach that secrete hydrochloric acid (HCl) and intrinsic factor. These cells are located in the gastric glands found in the lining of the fundus and body regions of the stomach. They contain an extensive secretory network of canaliculi from which the HCl is secreted by active transport into the stomach. The enzyme hydrogen potassium ATPase (H+/K+ ATPase) is unique to the parietal cells and transports the H+ against a concentration gradient of about 3 million to 1, which is the steepest ion gradient formed in the human body. Parietal cells are primarily regulated via histamine, acetylcholine and gastrin signalling from both central and local modulators.

Digestive enzymes are a group of enzymes that break down polymeric macromolecules into their smaller building blocks, in order to facilitate their absorption into the cells of the body. Digestive enzymes are found in the digestive tracts of animals and in the tracts of carnivorous plants, where they aid in the digestion of food, as well as inside cells, especially in their lysosomes, where they function to maintain cellular survival. Digestive enzymes of diverse specificities are found in the saliva secreted by the salivary glands, in the secretions of cells lining the stomach, in the pancreatic juice secreted by pancreatic exocrine cells, and in the secretions of cells lining the small and large intestines.
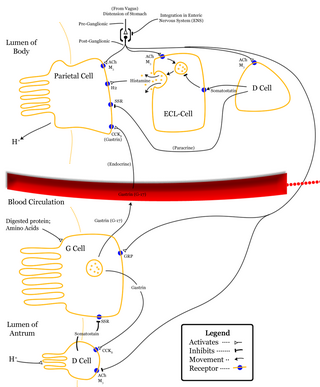
Enterochromaffin-like cells or ECL cells are a type of neuroendocrine cell found in the gastric glands of the gastric mucosa beneath the epithelium, in particular in the vicinity of parietal cells, that aid in the production of gastric acid via the release of histamine. They are also considered a type of enteroendocrine cell.

Enterochromaffin (EC) cells are a type of enteroendocrine cell, and neuroendocrine cell. They reside alongside the epithelium lining the lumen of the digestive tract and play a crucial role in gastrointestinal regulation, particularly intestinal motility and secretion. They were discovered by Nikolai Kulchitsky.
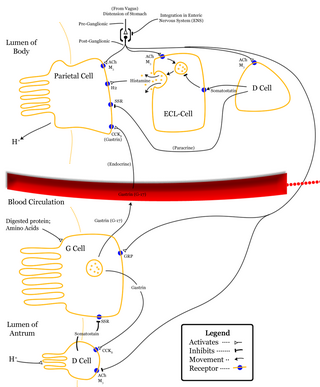
In anatomy, the G cell or gastrin cell is a type of cell in the stomach and duodenum that secretes gastrin. It works in conjunction with gastric chief cells and parietal cells. G cells are found deep within the pyloric glands of the stomach antrum, and occasionally in the pancreas and duodenum. The vagus nerve innervates the G cells. Gastrin-releasing peptide is released by the post-ganglionic fibers of the vagus nerve onto G cells during parasympathetic stimulation. The peptide hormone bombesin also stimulates gastrin from G cells. Gastrin-releasing peptide, as well as the presence of amino acids in the stomach, stimulates the release of gastrin from the G cells. Gastrin stimulates enterochromaffin-like cells to secrete histamine. Gastrin also targets parietal cells by increasing the amount of histamine and the direct stimulation by gastrin, causing the parietal cells to increase HCl secretion in the stomach. G-cells frequently express PD-L1 during homeostasis which protects them from Helicobacter pylori-induced immune destruction

Gastrinomas are neuroendocrine tumors (NETs), usually located in the duodenum or pancreas, that secrete gastrin and cause a clinical syndrome known as Zollinger–Ellison syndrome (ZES). A large number of gastrinomas develop in the pancreas or duodenum, with near-equal frequency, and approximately 10% arise as primary neoplasms in lymph nodes of the pancreaticoduodenal region.
Pancreatic juice is a liquid secreted by the pancreas, which contains a number of digestive enzymes, including trypsinogen, chymotrypsinogen, elastase, carboxypeptidase, pancreatic lipase, nucleases and amylase. The pancreas is located in the visceral region, and is a major part of the digestive system required for proper digestion and subsequent assimilation of macronutrient substances required for living.

The gastric glands are glands in the lining of the stomach that play an essential role in the process of digestion. All of the glands have mucus-secreting foveolar cells. Mucus lines the entire stomach, and protects the stomach lining from the effects of hydrochloric acid released from other cells in the glands.
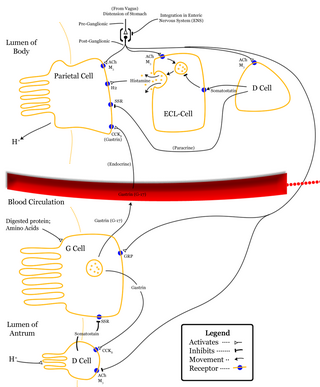
Vagovagal reflex refers to gastrointestinal tract reflex circuits where afferent and efferent fibers of the vagus nerve coordinate responses to gut stimuli via the dorsal vagal complex in the brain. The vagovagal reflex controls contraction of the gastrointestinal muscle layers in response to distension of the tract by food. This reflex also allows for the accommodation of large amounts of food in the gastrointestinal tracts.
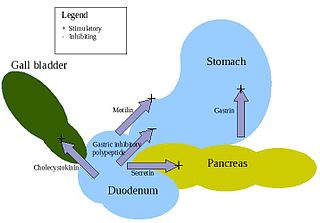
Enteroendocrine cells are specialized cells of the gastrointestinal tract and pancreas with endocrine function. They produce gastrointestinal hormones or peptides in response to various stimuli and release them into the bloodstream for systemic effect, diffuse them as local messengers, or transmit them to the enteric nervous system to activate nervous responses. Enteroendocrine cells of the intestine are the most numerous endocrine cells of the body. They constitute an enteric endocrine system as a subset of the endocrine system just as the enteric nervous system is a subset of the nervous system. In a sense they are known to act as chemoreceptors, initiating digestive actions and detecting harmful substances and initiating protective responses. Enteroendocrine cells are located in the stomach, in the intestine and in the pancreas. Microbiota play key roles in the intestinal immune and metabolic responses in these enteroendocrine cells via their fermentation product, acetate.
Gastrointestinal physiology is the branch of human physiology that addresses the physical function of the gastrointestinal (GI) tract. The function of the GI tract is to process ingested food by mechanical and chemical means, extract nutrients and excrete waste products. The GI tract is composed of the alimentary canal, that runs from the mouth to the anus, as well as the associated glands, chemicals, hormones, and enzymes that assist in digestion. The major processes that occur in the GI tract are: motility, secretion, regulation, digestion and circulation. The proper function and coordination of these processes are vital for maintaining good health by providing for the effective digestion and uptake of nutrients.
The proventriculus is part of the digestive system of birds. An analogous organ exists in invertebrates and insects.
The nervous system, and endocrine system collaborate in the digestive system to control gastric secretions, and motility associated with the movement of food throughout the gastrointestinal tract, including peristalsis, and segmentation contractions.

The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion. Digestion involves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body. The process of digestion has three stages: the cephalic phase, the gastric phase, and the intestinal phase.