Related Research Articles
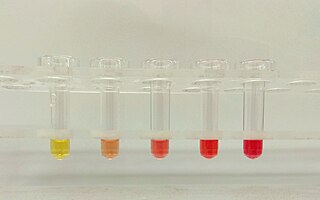
Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.
Serology is the scientific study of serum and other body fluids. In practice, the term usually refers to the diagnostic identification of antibodies in the serum. Such antibodies are typically formed in response to an infection, against other foreign proteins, or to one's own proteins. In either case, the procedure is simple.
The direct and indirect Coombs tests, also known as antiglobulin test (AGT), are blood tests used in immunohematology. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells they can cause anemia; this test can help clarify the condition. The indirect Coombs test detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells; the test can be carried out to diagnose reactions to a blood transfusion.
Warm antibody autoimmune hemolytic anemia (WAIHA) is the most common form of autoimmune haemolytic anemia. About half of the cases are of unknown cause, with the other half attributable to a predisposing condition or medications being taken. Contrary to cold autoimmune hemolytic anemia which happens in cold temperature (28–31 °C), WAIHA happens at body temperature.
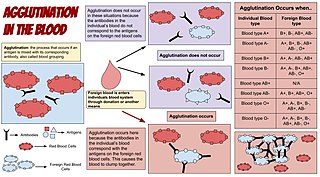
Agglutination is the clumping of particles. The word agglutination comes from the Latin agglutinare.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5–10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Paroxysmal cold hemoglobinuria (PCH) or Donath–Landsteiner hemolytic anemia (DLHA) is an autoimmune hemolytic anemia featured by complement-mediated intravascular hemolysis after cold exposure. It can present as an acute non-recurrent postinfectious event in children, or chronic relapsing episodes in adults with hematological malignancies or tertiary syphilis. Described by Julius Donath (1870–1950) and Karl Landsteiner (1868–1943) in 1904, PCH is one of the first clinical entities recognized as an autoimmune disorder.
In ABO hemolytic disease of the newborn maternal IgG antibodies with specificity for the ABO blood group system pass through the placenta to the fetal circulation where they can cause hemolysis of fetal red blood cells which can lead to fetal anemia and HDN. In contrast to Rh disease, about half of the cases of ABO HDN occur in a firstborn baby and ABO HDN does not become more severe after further pregnancies.
Cold agglutinin disease (CAD) is a rare autoimmune disease characterized by the presence of high concentrations of circulating cold sensitive antibodies, usually IgM and autoantibodies that are also active at temperatures below 30 °C (86 °F), directed against red blood cells, causing them to agglutinate and undergo lysis. It is a form of autoimmune hemolytic anemia, specifically one in which antibodies bind red blood cells only at low body temperatures, typically 28–31 °C.
The Kell antigen system is a human blood group system, that is, a group of antigens on the human red blood cell surface which are important determinants of blood type and are targets for autoimmune or alloimmune diseases which destroy red blood cells. The Kell antigens are K, k, Kpa, Kpb, Jsa and Jsb. The Kell antigens are peptides found within the Kell protein, a 93-kilodalton transmembrane zinc-dependent endopeptidase which is responsible for cleaving endothelin-3.

The Ii antigen system is a human blood group system based upon a gene on chromosome 6 and consisting of the I antigen and the i antigen. The I antigen is normally present on the cell membrane of red blood cells in all adults, while the i antigen is present in fetuses and newborns.
Hematologic diseases are disorders which primarily affect the blood & blood-forming organs. Hematologic diseases include rare genetic disorders, anemia, HIV, sickle cell disease & complications from chemotherapy or transfusions.
Acquired hemolytic anemia can be divided into immune and non-immune mediated forms of hemolytic anemia.

Drug-induced autoimmune hemolytic anemia also known as Drug-induced immune hemolytic anemia (DIIHA) is a rare cause of hemolytic anemia. It is difficult to differentiate from other forms of anemia which can lead to delays in diagnosis and treatment. Many different types of antibiotics can cause DIIHA and discontinuing the offending medication is the first line of treatment. DIIHA has is estimated to affect one to two people per million worldwide.

In hematology, red cell agglutination or autoagglutination is a phenomenon in which red blood cells clump together, forming aggregates. It is caused by the surface of the red cells being coated with antibodies. This often occurs in cold agglutinin disease, a type of autoimmune hemolytic anemia in which people produce antibodies that bind to their red blood cells at cold temperatures and destroy them. People may develop cold agglutinins from lymphoproliferative disorders, from infection with Mycoplasma pneumoniae or Epstein–Barr virus, or idiopathically. Red cell agglutination can also occur in paroxysmal nocturnal hemoglobinuria and warm autoimmune hemolytic anemia. In cases of red cell agglutination, the direct antiglobulin test can be used to demonstrate the presence of antibodies bound to the red cells.

Fostamatinib, sold under the brand names Tavalisse and Tavlesse, is a tyrosine kinase inhibitor medication for the treatment of chronic immune thrombocytopenia (ITP). The drug is administered by mouth.
Cold autoimmune hemolytic anemia caused by cold-reacting antibodies. Autoantibodies that bind to the erythrocyte membrane leading to premature erythrocyte destruction (hemolysis) characterize autoimmune hemolytic anemia.
Sutimlimab, sold under the brand name Enjaymo, is a monoclonal antibody that is used to treat adults with cold agglutinin disease (CAD). It is given by intravenous infusion. Sutimlimab prevents complement-enhanced activation of autoimmune human B cells in vitro.
Cold sensitive antibodies (CSA) are antibodies sensitive to cold temperature. Some cold sensitive antibodies are pathological and can lead to blood disorder. These pathological cold sensitive antibodies include cold agglutinins, Donath–Landsteiner antibodies, and cryoglobulins which are the culprits of cold agglutinin disease, paroxysmal cold hemoglobinuria in the process of Donath–Landsteiner hemolytic anemia, and vasculitis, respectively.
References
- 1 2 Mayer, Beate; Yürek, Salih; Kiesewetter, Holger; Salama, Abdulgabar (2008). "Mixed-type autoimmune hemolytic anemia: differential diagnosis and a critical review of reported cases". Transfusion. Wiley. 48 (10): 2229–2234. doi:10.1111/j.1537-2995.2008.01805.x. ISSN 0041-1132. PMID 18564390. S2CID 46182439.
- ↑ Berentsen, Sigbjørn; Sundic, Tatjana (2015-01-29). "Red Blood Cell Destruction in Autoimmune Hemolytic Anemia: Role of Complement and Potential New Targets for Therapy". BioMed Research International. Hindawi Limited. 2015: 363278. doi: 10.1155/2015/363278 . ISSN 2314-6133. PMC 4326213 . PMID 25705656.
- ↑ "Orphanet: Autoimmune hemolytic anemia, warm type". Orphanet. 2019-02-14. Retrieved 2019-02-15.
- ↑ Das, SudiptaSekhar; Chakrabarty, Ritam; Zaman, RU (2018). "Immunohematological and clinical characterizations of mixed autoimmune hemolytic anemia". Asian Journal of Transfusion Science. Medknow. 12 (2): 99–104. doi: 10.4103/ajts.ajts_105_17 . ISSN 0973-6247. PMC 6327768 . PMID 30692792.
- ↑ Gupta, Shilpi; Szerszen, Anita; Nakhl, Fadi; Varma, Seema; Gottesman, Aaron; Forte, Frank; Dhar, Meekoo (2011-04-19). "Severe refractory autoimmune hemolytic anemia with both warm and cold autoantibodies that responded completely to a single cycle of rituximab: a case report". Journal of Medical Case Reports. Springer Nature. 5 (1): 156. doi: 10.1186/1752-1947-5-156 . ISSN 1752-1947. PMC 3096571 . PMID 21504611.
- 1 2 Berentsen, Sigbjørn; Sundic, Tatjana (2015-01-29). "Red Blood Cell Destruction in Autoimmune Hemolytic Anemia: Role of Complement and Potential New Targets for Therapy". BioMed Research International. Hindawi Limited. 2015. 363278-1–363278-11. doi: 10.1155/2015/363278 . ISSN 2314-6133. PMC 4326213 . PMID 25705656.
- ↑ Berentsen, S; Ulvestad, E; Langholm, R; Beiske, K; Hjorth-Hansen, H; Ghanima, W; Sørbø, JH; Tjønnfjord, GE (2006). "Primary chronic cold agglutinin disease: a population based clinical study of 86 patients". Haematologica. 91 (4): 460–6. ISSN 0390-6078. PMID 16585012.