Related Research Articles

Agar, or agar-agar, is a jelly-like substance consisting of polysaccharides obtained from the cell walls of some species of red algae, primarily from ogonori (Gracilaria) and "tengusa" (Gelidiaceae).

Staphylococcus aureus is a Gram-positive round-shaped bacterium, a member of the Firmicutes, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin. It is often positive for catalase and nitrate reduction and is a facultative anaerobe that can grow without the need for oxygen. Although S. aureus usually acts as a commensal of the human microbiota it can also become an opportunistic pathogen, being a common cause of skin infections including abscesses, respiratory infections such as sinusitis, and food poisoning. Pathogenic strains often promote infections by producing virulence factors such as potent protein toxins, and the expression of a cell-surface protein that binds and inactivates antibodies. The emergence of antibiotic-resistant strains of S. aureus such as methicillin-resistant S. aureus (MRSA) is a worldwide problem in clinical medicine. Despite much research and development, no vaccine for S. aureus has been approved.

An agar plate is a Petri dish that contains a growth medium solidified with agar, used to culture microorganisms. Sometimes selective compounds are added to influence growth, such as antibiotics.

A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia or fungemia, which in severe cases may result in sepsis. By culturing the blood, microbes can be identified and tested for resistance to antimicrobial drugs, which allows clinicians to provide an effective treatment.

A growth medium or culture medium is a solid, liquid, or semi-solid designed to support the growth of a population of microorganisms or cells via the process of cell proliferation or small plants like the moss Physcomitrella patens. Different types of media are used for growing different types of cells.

MacConkey agar is a selective and differential culture medium for bacteria. It is designed to selectively isolate Gram-negative and enteric bacteria and differentiate them based on lactose fermentation. Lactose fermenters turn red or pink on McConkey agar, and nonfermenters do not change color. The media inhibits growth of Gram-positive organisms with crystal violet and bile salts, allowing for the selection and isolation of gram-negative bacteria. The media detects lactose fermentation by enteric bacteria with the pH indicator neutral red.

Staphylococcus haemolyticus is a member of the coagulase-negative staphylococci (CoNS). It is part of the skin flora of humans, and its largest populations are usually found at the axillae, perineum, and inguinal areas. S. haemolyticus also colonizes primates and domestic animals. It is a well-known opportunistic pathogen, and is the second-most frequently isolated CoNS. Infections can be localized or systemic, and are often associated with the insertion of medical devices. The highly antibiotic-resistant phenotype and ability to form biofilms make S. haemolyticus a difficult pathogen to treat. Its most closely-related species if Staphylococcus borealis.
Staphylococcus hominis is a coagulase-negative member of the bacterial genus Staphylococcus, consisting of Gram-positive, spherical cells in clusters. It occurs very commonly as a harmless commensal on human and animal skin and is known for producing thioalcohol compounds that contribute to body odour. Like many other coagulase-negative staphylococci, S. hominis may occasionally cause infection in patients whose immune systems are compromised, for example by chemotherapy or predisposing illness.

Haemophilus is a genus of Gram-negative, pleomorphic, coccobacilli bacteria belonging to the family Pasteurellaceae. While Haemophilus bacteria are typically small coccobacilli, they are categorized as pleomorphic bacteria because of the wide range of shapes they occasionally assume. These organisms inhabit the mucous membranes of the upper respiratory tract, mouth, vagina, and intestinal tract. The genus includes commensal organisms along with some significant pathogenic species such as H. influenzae—a cause of sepsis and bacterial meningitis in young children—and H. ducreyi, the causative agent of chancroid. All members are either aerobic or facultatively anaerobic. This genus has been found to be part of the salivary microbiome.

Staphylococcus epidermidis is a Gram-positive bacterium, and one of over 40 species belonging to the genus Staphylococcus. It is part of the normal human flora, typically the skin flora, and less commonly the mucosal flora and also found in marine sponges. It is a facultative anaerobic bacteria. Although S. epidermidis is not usually pathogenic, patients with compromised immune systems are at risk of developing infection. These infections are generally hospital-acquired. S. epidermidis is a particular concern for people with catheters or other surgical implants because it is known to form biofilms that grow on these devices. Being part of the normal skin flora, S. epidermidis is a frequent contaminant of specimens sent to the diagnostic laboratory.

Antibiotic sensitivity testing or antibiotic susceptibility testing is the measurement of the susceptibility of bacteria to antibiotics. It is used because bacteria may have resistance to some antibiotics. Sensitivity testing results can allow a clinician to change the choice of antibiotics from empiric therapy, which is when an antibiotic is selected based on clinical suspicion about the site of an infection and common causative bacteria, to directed therapy, in which the choice of antibiotic is based on knowledge of the organism and its sensitivities.

Mannitol salt agar or MSA is a commonly used selective and differential growth medium in microbiology. It encourages the growth of a group of certain bacteria while inhibiting the growth of others. This medium is important in medical laboratories as one method of distinguishing pathogenic microbes in a short period of time. It contains a high concentration of salt (NaCl) which is inhibitory to most bacteria - making MSA selective against most Gram-negative and selective for some Gram-positive bacteria that tolerate high salt concentrations. It is also a differential medium for mannitol-fermenting staphylococci, containing carbohydrate mannitol and the indicator phenol red, a pH indicator for detecting acid produced by mannitol-fermenting staphylococci. Staphylococcus aureus produces yellow colonies with yellow zones, whereas other coagulase-negative staphylococci produce small pink or red colonies with no colour change to the medium. If an organism can ferment mannitol, an acidic byproduct is formed that causes the phenol red in the agar to turn yellow. It is used for the selective isolation of presumptive pathogenic (pp) Staphylococcus species.

Etest is a way of determining antimicrobial sensitivity by placing a strip impregnated with antimicrobials onto an agar plate. A strain of bacterium or fungus will not grow near a concentration of antibiotic or antifungal if it is sensitive. For some microbial and antimicrobial combinations, the results can be used to determine a minimum inhibitory concentration (MIC). Etest is a proprietary system manufactured by bioMérieux. It is a laboratory test used in healthcare settings to help guide physicians by indicating what concentration of antimicrobial could successfully be used to treat patients' infections.
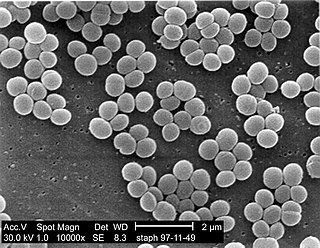
Staphylococcus is a genus of Gram-positive bacteria in the family Staphylococcaceae from the order Bacillales. Under the microscope, they appear spherical (cocci), and form in grape-like clusters. Staphylococcus species are facultative anaerobic organisms.
Staphylococcus succinus is a Gram-positive coccoid bacterium belonging to the genus Staphylococcus.

Staphylococcus hyicus is a Gram-positive, facultatively anaerobic bacterium in the genus Staphylococcus. It consists of clustered cocci and forms white circular colonies when grown on blood agar. S. hyicus is a known animal pathogen. It causes disease in poultry, cattle, horses, and pigs. Most notably, it is the agent that causes porcine exudative epidermitis, also known as greasy pig disease, in piglets. S. hyicus is generally considered to not be zoonotic, however it has been shown to be able to cause bacteremia and sepsis in humans.
Staphylococcus schleiferi is a Gram-positive, cocci-shaped bacterium of the family Staphylococcaceae. It is facultatively anaerobic, coagulase-variable, and can be readily cultured on blood agar where the bacterium tends to form opaque, non-pigmented colonies and beta (β) hemolysis. There exists two subspecies under the species S. schleiferi: Staphylococcus schleiferi subsp. schleiferi and Staphylococcus schleiferi subsp. coagulans.
Staphylococcus pseudintermedius is a gram positive coccus bacteria of the genus Staphylococcus found worldwide. It is primarily a pathogen for domestic animals, but has been known to affect humans as well.S. pseudintermedius is an opportunistic pathogen that secretes immune modulating virulence factors, has many adhesion factors, and the potential to create biofilms, all of which help to determine the pathogenicity of the bacterium. Diagnoses of Staphylococcus pseudintermedius have traditionally been made using cytology, plating, and biochemical tests. More recently, molecular technologies like MALDI-TOF, DNA hybridization and PCR have become preferred over biochemical tests for their more rapid and accurate identifications. This includes the identification and diagnosis of antibiotic resistant strains.
Diagnostic microbiology is the study of microbial identification. Since the discovery of the germ theory of disease, scientists have been finding ways to harvest specific organisms. Using methods such as differential media or genome sequencing, physicians and scientists can observe novel functions in organisms for more effective and accurate diagnosis of organisms. Methods used in diagnostic microbiology are often used to take advantage of a particular difference in organisms and attain information about what species it can be identified as, which is often through a reference of previous studies. New studies provide information that others can reference so that scientists can attain a basic understanding of the organism they are examining.

In microbiology, colonial morphology refers to the visual appearance of bacterial or fungal colonies on an agar plate. Examining colonial morphology is the first step in the identification of an unknown microbe. The systematic assessment of the colonies' appearance, focusing on aspects like size, shape, colour, opacity, and consistency, provides clues to the identity of the organism, allowing microbiologists to select appropriate tests to provide a definitive identification.
References
- ↑ Janda, W.M.; K. Ristow; D. Novak (September 1994). "Evaluation of RapiDEC Staph for Identification of Staphylococcus aureus, Staphylococcus epidermidis, and Staphylococcus saprophyticus". Journal of Clinical Microbiology. 32 (9): 2056–2059. PMC 263941 . PMID 7814525.
- ↑ Geary, C.; M. Stevens (October 1989). "Detection of phosphatase production by Staphylococcus species: a new method". Med Lab Sci. 46 (4): 291–294. PMID 2559282.